Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic autoimmune disease with considerable clinical and molecular heterogeneity. Significant disparities exist in SLE, with minority populations experiencing higher prevalence, increased disease severity, and earlier mortality. Recent studies suggest that adverse social determinants of health may contribute to these disparities. This study evaluated the association between neighborhood-level social vulnerability, measured by the Social Vulnerability Index (SVI), and disease severity, clinical manifestations, and early mortality among female SLE patients in the Lupus Family Registry and Repository (LFRR).
Methods: The LFRR is a large, cross-sectional cohort of SLE patients and their unaffected family members. Patients met ACR 1997 classification criteria for SLE, were female, and had available residential addresses for geocoding (n=3,033). Of those patients, 1,091 were deceased prior to 2024 and included in the early mortality analysis. Disease severity was assessed using the Montgomery Lupus Severity Index (LSI; high severity defined as LSI >7). SVI percentiles (range 0-1) were categorized as high (percentile >0.50) or low (≤ 0.50) vulnerability. Early mortality was defined as death before the average age of death in the US population from 1999-2020, stratified by sex and race. Descriptive statistics and separate logistic regression models were used to evaluate associations with SVI factors, LSI, ACR criteria, and lupus nephritis (LN).
Results: Consistent with previous studies, we observed significant racial differences in disease severity, and clinical manifestations along with higher percentages of early mortality (Table 1 and Figure 1). In univariate analyses, high SVI was associated with increased odds of certain ACR criteria and LSI (Figure 1A). However, these associations were no longer statistically significant after adjusting for race (Figure 1B). Racial differences in disease severity and organ involvement persisted even after accounting for SVI (Figure 1). Patients who died early had significantly higher SVI scores for low economic and household instability factors, indicating greater social vulnerability (Figure 2). Notably, these factors remained significantly associated with early mortality following adjustment for race, sex and high LSI (Figure 2).
Conclusion: In the LFRR, neighborhood-level social vulnerability was not associated with SLE severity or organ involvement after accounting for race. Persistent racial disparities in SLE severity and manifestations suggest that factors beyond area-level vulnerability, including genetic, epigenetic, and individual-level environmental exposures, may play a more substantial role. Social vulnerability, particularly low economic and household instability factors, was significantly associated with early mortality.
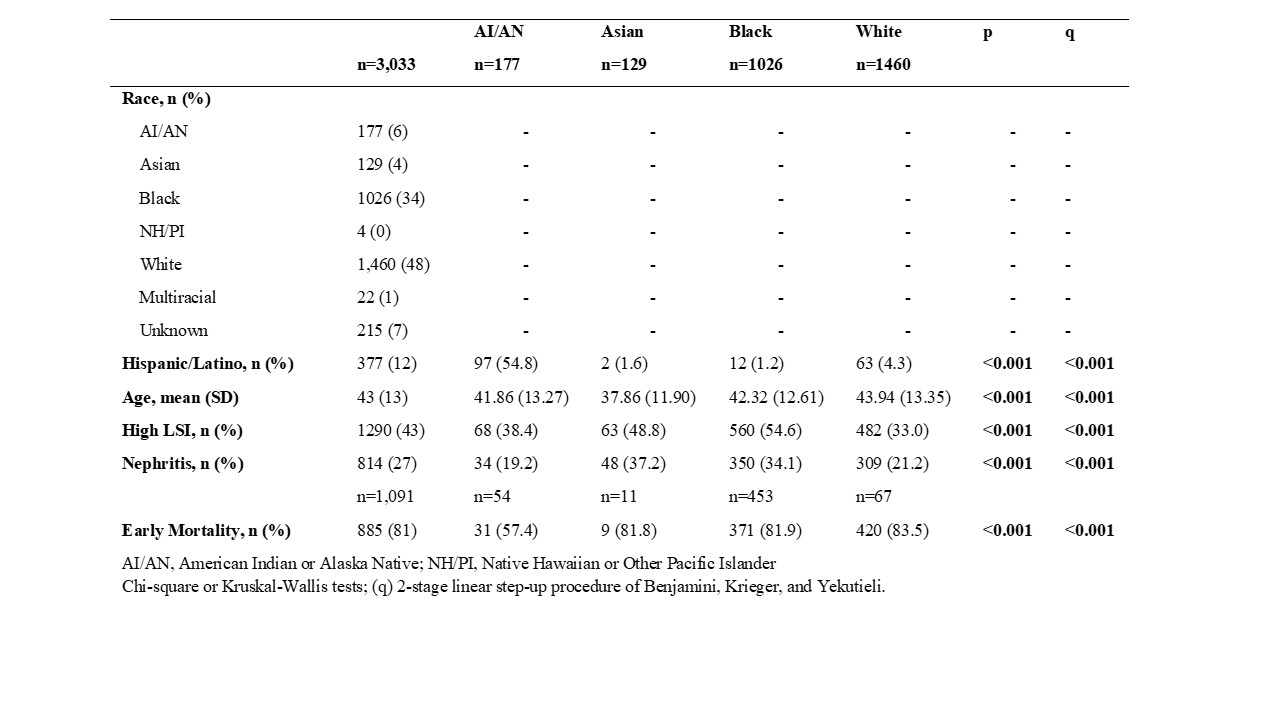 Table 1: Demographic and clinical characteristics
Table 1: Demographic and clinical characteristics
.jpg) Figure 1: Associations of social vulnerability index and self-reported race with SLE disease severity and clinical manifestations. (A) Univariate and (B) multivariate logistic regression models for associations with different clinical characteristics. The multivariate model incorporates self-reported race categories and low vs high SVI.
Figure 1: Associations of social vulnerability index and self-reported race with SLE disease severity and clinical manifestations. (A) Univariate and (B) multivariate logistic regression models for associations with different clinical characteristics. The multivariate model incorporates self-reported race categories and low vs high SVI.
.jpg) Figure 2: Associations of social vulnerability index with early mortality in SLE; multivariate logistic regression models for associations with different SVI factors. The multivariate model incorporates self-reported race categories, sex, high LSI, and low vs high SVI.
Figure 2: Associations of social vulnerability index with early mortality in SLE; multivariate logistic regression models for associations with different SVI factors. The multivariate model incorporates self-reported race categories, sex, high LSI, and low vs high SVI.
To cite this abstract in AMA style:
Reed Z, Wagner C, Howard X, Cammarata-Mouchtouris A, ALE06 Clinical S, DeJager W, James J. Impact of Neighborhood-Level Social Vulnerability on Disease Severity, Clinical Manifestations, and Early Mortality in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-neighborhood-level-social-vulnerability-on-disease-severity-clinical-manifestations-and-early-mortality-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-neighborhood-level-social-vulnerability-on-disease-severity-clinical-manifestations-and-early-mortality-in-systemic-lupus-erythematosus/
