Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Studies have demonstrated that socioeconomic status (SES) significantly influences outcomes of patients with SLE.1 Traditionally, tools such as income, education, occupation, and housing have been used as markers of SES, but these are useful for epidemiological purposes or for large community-wide interventions, and less helpful in identifying specific vulnerable patients. The Area Deprivation Index (ADI) is a validated tool based on individual patients’ home addresses and incorporates multiple indicators of SES disadvantage into a single index; thereby, quantifying disadvantage on a neighborhood level.2,3 Our study aims to assess the impact of ADI on SLE patient outcomes in the Bronx, the poorest urban community in the United States.
Methods: Patients meeting the 1997 ACR SLE classification criteria and enrolled in the Einstein Lupus Cohort (Montefiore Medical Center, Bronx, NY) from 2018-2023 were identified. Data was collected retrospectively via chart review starting at Year 0 (Y0), defined as the year of the initial rheumatology visit in the electronic health record (EHR) system. Data points were collected every 2 years until Year 6 (Y6). Outpatient rheumatology visits and lab tests at Y0, Y2, Y4, and Y6 were used to calculate SLEDAI and SLICC Damage Index (SDI). State-specific ADI deciles were derived from patients’ most recent home addresses, with higher deciles indicating greater disadvantage. Data is presented as median(IQR). Mann-Whitney U/Kruskal-Wallis Tests, with Dunnett’s Correction for multiple comparisons, were used for data analysis.
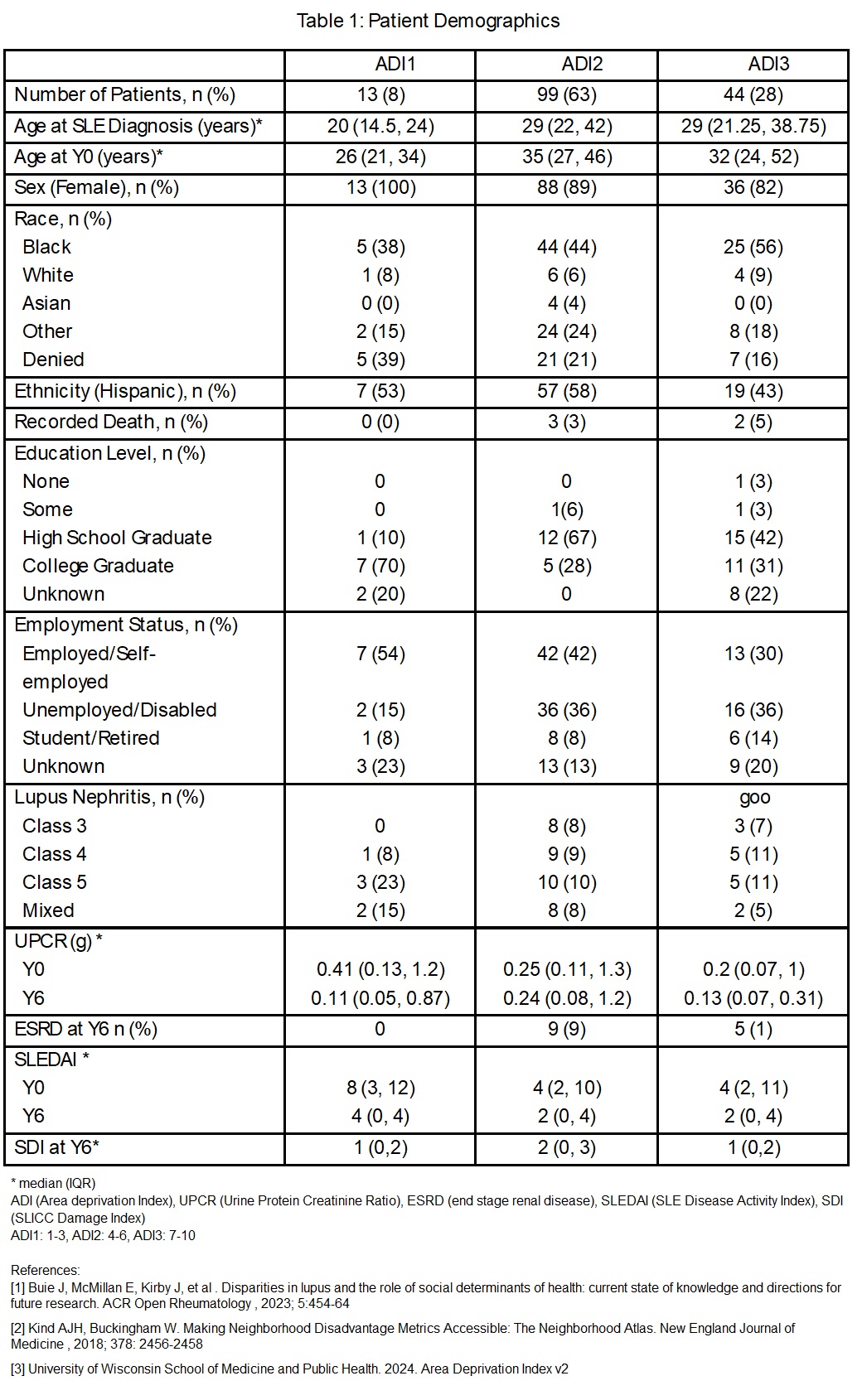
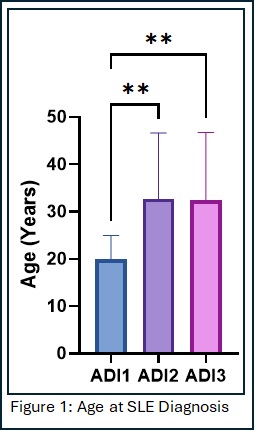
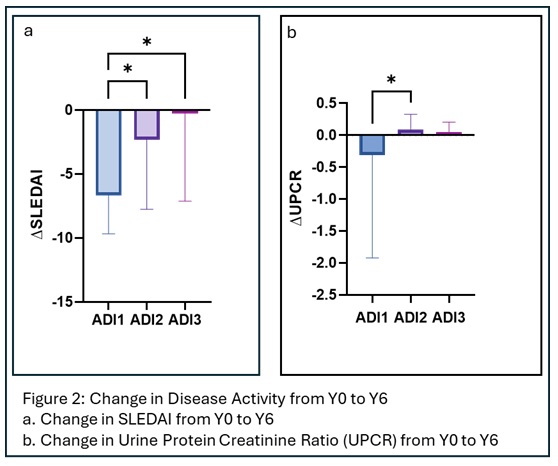
Results: Out of 156 patients, 8% were categorized in ADI1 (state deciles 1-3, most advantageous), 63% in ADI2 (deciles 4-6), and 28% in ADI3 (deciles 7-10) (Table 1). Education levels were significantly different between the ADI groups (p=0.025), while there was no significant difference in race and ethnicity. Patients with ADI1 were diagnosed at an earlier age than those with ADI2 and ADI3 [age 20 (14.5, 24) vs 29 (22, 42), p=0.001, and 29 (21, 39), p=0.004, respectively] (Fig. 1). By Y6, there were significant differences in change in SLEDAI (∆SLEDAI) between ADI1 vs ADI2 [-8 (-8.5, -3.5) vs -2 (-4,0), p=0.04] and ADI1 vs ADI3 [-8 (-8.5, -3.5) vs 0 (-4,2), p=0.02] (Fig. 2A). In addition, there was a significant difference in change in proteinuria between the ADI groups by Y6 (-0.31 (-1.9, -0.12) vs 0.09 (-0.04, 0.33) vs 0.05 (-0.07, 0.21), p=0.043) (Fig. 2B). No significant difference in SDI was noted among the three groups.
Conclusion: Patients residing in areas with higher ADI are diagnosed with SLE later, and achieve worse outcomes compared to those in areas with lower ADI. Specifically, they experience ongoing disease activity despite years of medical management. While deeper exploration of the factors causing these disparities is necessary, our findings suggest that early identification and targeted interventions for patients with higher ADI may be warranted.
To cite this abstract in AMA style:
Ramu A, Shafik J, Ashrafi M, Allen J, Brennan K, Schwartz N. Impact of Neighborhood Area Deprivation Index on Outcomes in Lupus Patients in Bronx, NY [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-neighborhood-area-deprivation-index-on-outcomes-in-lupus-patients-in-bronx-ny/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-neighborhood-area-deprivation-index-on-outcomes-in-lupus-patients-in-bronx-ny/