Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: To evaluate the impact of multimorbidity on the effectiveness of targeted synthetic and biologic disease-modifying antirheumatic drug (ts/bDMARD), in patients with rheumatoid arthritis in a two-year follow-up.
Methods: In this analysis we included all patients with rheumatoid arthritis (RA) registered from 2016 to April 2024 in Biobadamex. Patients were categorized based on multimorbidity status at baseline, defined as a Charlson Comorbidity index (CCI) score ≥ 3. A linear regression model, adjusted for sex and age, was employed to compare the absolute DAS28 score over time after ts/bDMARD initiation between the two groups.
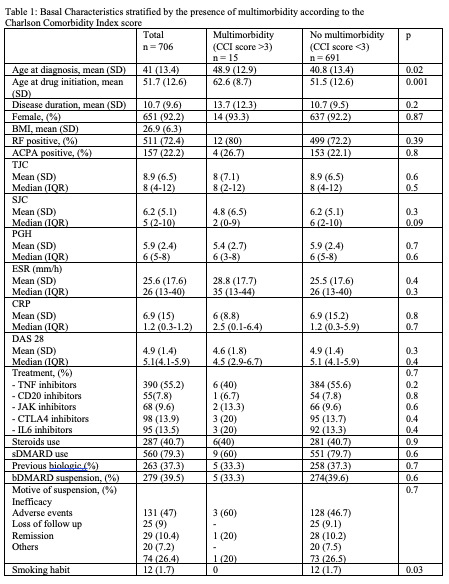
Results: A total of 706 patients with rheumatoid arthritis were included in the analysis (Table 1), mean age at diagnosis was 41 (SD 13.4) years, age at drug initiation was 51.7 (SD 12.6) and disease duration until ts/bDMARD initiation was 10.7 (SD 9.6). The most used bDMARD were TNF inhibitors (55.2%) followed by CTLA4 inhibitors (13.9%).
The most prevalent comorbidities among the patients were uncomplicated diabetes mellitus (9.8%), mild liver disease (1.8%) and solid tumor and peptic ulcer (1.3% each)
A total of 15 patients (2.12%) had multimorbidity represented by a CCI > 3. These patients had a higher age at diagnosis [48.9 (SD 12.9) vs 40.8 (13.4), p = 0.02] and higher age at drug initiation [51.7 (12.6) vs 51.5 (12.6), p = 0.001). C reactive protein [6 (8.8) vs 6.9 (15.2), p = 0.8] and disease activity measured by DAS28 index was lower in the multimorbidity group [4.6 (1.8) vs 4.9 (1.4), p = 0.3), but this had no statistical significance. TNF inhibitors were the most prescribed bDMARD, but in lower proportion than no multimorbidity patients. Steroids use was similar in both groups and sDMARD use was lower in the multimorbididy group.
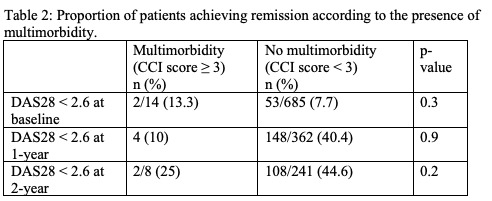
The proportion of patients that achieved remission (Table 2) was higher in the no multimorbidity group at one year (40.4% vs 10%, p = 0.9) and two years (44.6% vs 25%, p = 0.2). When followed in time we observed the reduction of DAS 28 over the first two years (Figure 1) with similar reduction in both groups the first year and higher reduction in the no multimorbidity group the second year, with no statistical significance (p = 0.4).
Conclusion: In this study we found that multimorbidity seems to have an impact on the effectiveness of treatment in RA patients, with a higher DAS28 scores in a two-year follow-up. As our multimorbidity group was small we consider this may affected the statistical significance of our results so the m which is higher in the second year of follow up.
To cite this abstract in AMA style:
Rivera Teran V, Vega Morales D, Colunga Pedraza I, Sicsik Ayala S, Castillo Ortiz A, Saavedra Salinas M, Miranda Hernández D, Irazoque Palazuelos F, Casasola Vargas J, Muñoz Monroy O, Carrillo Vazquez S, Merayo Chalico j, Guaracha Basañez G, Torres Valdez E, Valdés Corona L, Peña Ayala A, Durán Barragán S, Ramos Sánchez A, Paz Viscarra A, Zamora Tehozol E, Xibillé Friedman D, Torres Ruiz J. Impact of Multimorbidity on Targeted Synthetic and Biologic Disease-modifying Antirheumatic Drug (ts/bDMARD) Effectiveness in Patients with Rheumatoid Arthritis: A Two Year Follow-up Study from Mexican Adverse Events Registry BIOADAMEX [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-multimorbidity-on-targeted-synthetic-and-biologic-disease-modifying-antirheumatic-drug-ts-bdmard-effectiveness-in-patients-with-rheumatoid-arthritis-a-two-year-follow-up-study-from-mexica/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-multimorbidity-on-targeted-synthetic-and-biologic-disease-modifying-antirheumatic-drug-ts-bdmard-effectiveness-in-patients-with-rheumatoid-arthritis-a-two-year-follow-up-study-from-mexica/