Session Information
Date: Sunday, October 21, 2018
Title: Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I: Comorbidities
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: In early atherogenesis inflammation drives and co-localizes with intimal calcification. In chronic, advanced plaques inflammation and calcification are inversely correlated and spatially distinct; advanced calcification is considered a stabilizing physiologic process rendering plaques less prone to rupture. We evaluated the role of inflammation, biologic treatments and cardiac risk factors on the de-novo generation and progression of advanced, calcified coronary plaques (CP) in patients with rheumatoid arthritis (RA).
Methods: Ninety-nine participants with a baseline non-invasive evaluation of coronary anatomy with computed tomography angiography (CCTA) underwent a repeat assessment within 83±3.6 months. Coronary lesions were counted and defined as non-calcified (NCP), mixed (MP) or calcified (CP). The prevalence, number, stenotic severity and burden of individual CP plaques was recorded. Patients were classified into three groups according to plaque disposition: CP-negative (no CP at any time), CP-positive (CP present at both times), and new-CP (absent at baseline, present at follow-up). A Multinomial logistic regression model evaluated predictors independently associated with patient classification into the CP-positive or New-CP groups compared to the CP negative group.
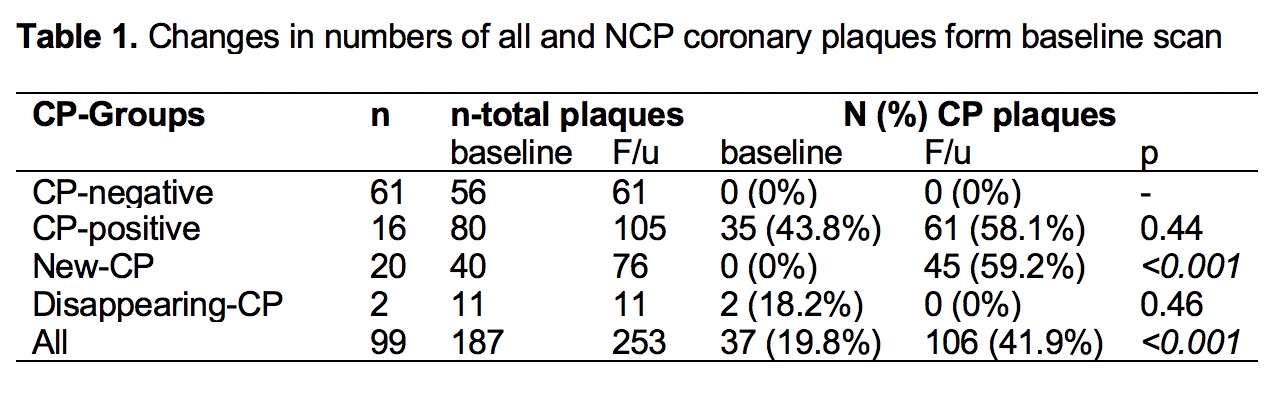
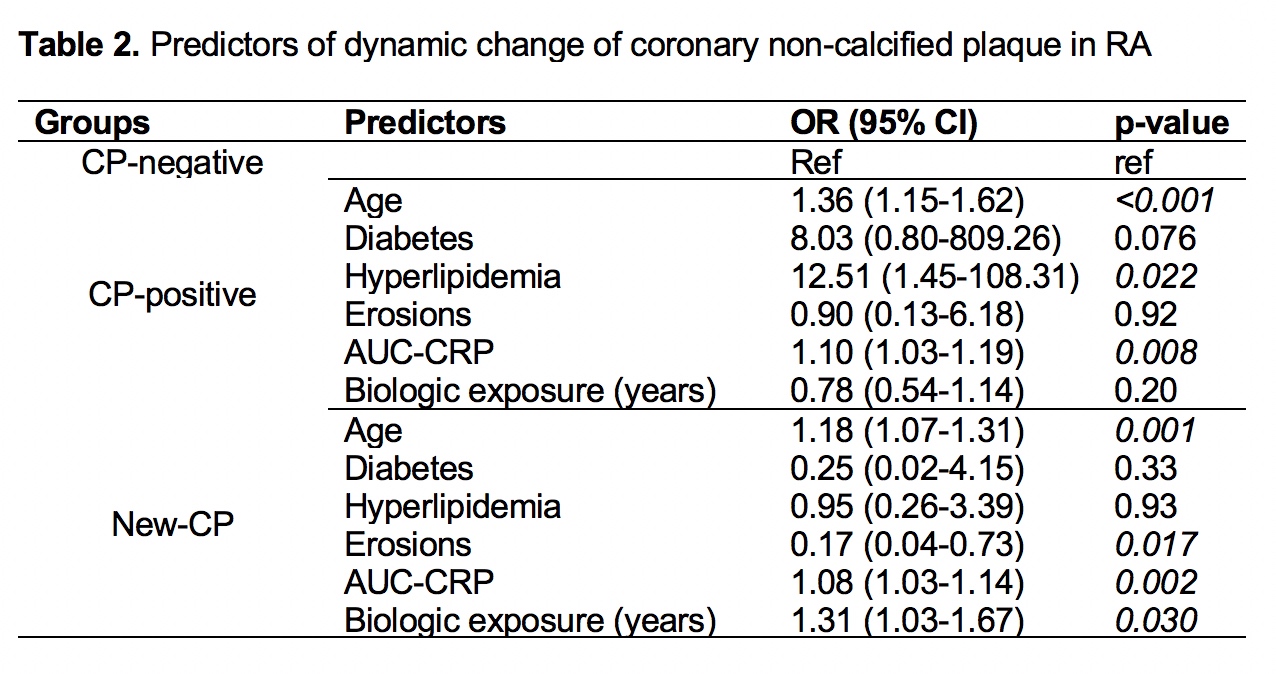
Results: CP prevalence was higher at follow-up compared to baseline (42.3% vs. 19.8%, p<0.001, table 1); 21 of 99 (21%) patients developed new CP lesions. In the CP-positive group, 43% of the lesions at follow-up were unchanged from baseline,16% derived from progression of MP, 3% from NCP and 23% were incident CP lesions. In the New-CP group, 73% of lesions were incident CP, 13% derived from NCP and 13% from MP. CP-positive patients were older, with greater baseline hyperlipidemia and higher inflammatory burden [area under the curve for c-reactive protein (AUC-CRP), p=0.008] compared to the CP-negative ones (table 2). New CP subjects were older, had greater frequency of baseline erosions, higher inflammatory burden (p=0.002) and lengthier biologic exposure (p=0.015) vs. the CP-negative group.
Conclusion: Higher inflammatory burden promotes generation, maturation and early calcification of coronary plaques in patients with RA. Higher duration of biologic exposure, through systemic and/ or local inflammatory control, fosters advanced calcification and stabilization of atherosclerotic plaques.
To cite this abstract in AMA style:
Karpouzas G, Ormseth S, Hernandez E, Budoff M. Impact of Inflammation and Biologic Treatments on Generation and Progression to Advanced Calcified Coronary Plaques in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/impact-of-inflammation-and-biologic-treatments-on-generation-and-progression-to-advanced-calcified-coronary-plaques-in-rheumatoid-arthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-inflammation-and-biologic-treatments-on-generation-and-progression-to-advanced-calcified-coronary-plaques-in-rheumatoid-arthritis/