Session Information
Date: Monday, November 18, 2024
Title: SLE – Treatment Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The administration of hydroxychloroquine-sulphate (HCQ) can lead to the risk of QTc prolongation and cardiac arrhythmias. We evaluated the HCQ concentration and the incidence of QTc prolongation among patients with systemic autoimmune diseases treated with HCQ for at least 1 year.
Methods: We studied 108 subjects with different systemic autoimmune diseases treated with HCQ at doses ranging from 200-400 mg per day or more than 1 year. Additionally, we included 56 subjects, matched for age and sex distributions, who had not received HCQ treatment as control group. HCQ concentration was measured using liquid chromatography, and QTc intervals were evaluated using established guidelines. The primary outcome measure sought was a QTc interval > 440 mg, considered pathological.
In patients with SARD was collected: 1) Epidemiological data: age, sex, weight, concomitant diseases, current treatment. 2) SARD: diagnosis, year of diagnosis, disease evolution time, clinical and autoimmunity data, treatment and dose. 3) HCQ: timen in treatment, toxicity, symptoms and serum level. 4) ECG: QTc interval and heart rate (HR).
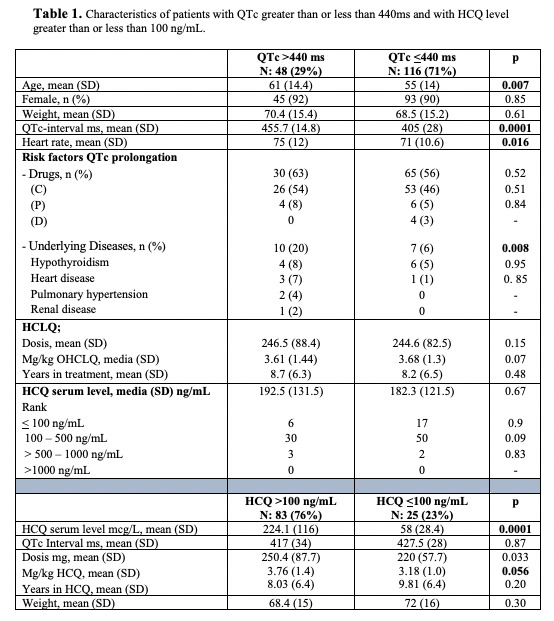
Results: The mean age of the patients in the total population was 55 years [range: 25-92; SD ±14], with 90% being women. The mean duration of HCQ therapy was 8±6,4 years, at a mean dose of 245±83.8mg and 3.7±1.3mg/kg/day of HCQ. Among those treated with HCQ, 39 (37%) individuals showed QTc interval > 440 ms compared with 9 (16%) in the control group (p= 0,49). There was no difference in serum HCQ concentrations between patients with QTc prolongation (192.5 ± 131.5 ng/mL) and those with normal QTc interval (182.3 ± 121.5 ng/mL; p=0.67). Patients with QTc prolongation had a higher frequency of underlying diseases associated with QTc prolongation than patients with normal QTc (20% vs 6%; p=0.004). The use of drugs with potential risk was not associated with QTc prolongation.
Among patients with HCQ level >100 ng/mL (n: 83/76%) vs <100 ng/mL (n: 25/23%), serum level (224.1 ng/mL [116] vs 58 [20.4], p< 0.0001), and dose of HCQ in mg/kg (3.76 [1.4] vs 3.18 [1.0], p=0.05), is significantly higher at levels >100 mcg/L. No relationship was observed between the HCQ level and the QTc result.
Conclusion: In patients with EAS treated with maintenance doses of 200-400 mg of HCQ per day and with weight-adjusted mean doses of 3.7 mg/kg/day: 1) The serum level of HCQ is not related to the prolongation of the interval QTc of the ECG. 2) QTc is significantly related to age, heart rate and underlying diseases. 3) Patients on long-term treatment with HCQ also receive other common drugs that can influence QTc, however, it does not seem to cause serious symptoms of interest. 4) EAS per se does not affect the QTc result.
To cite this abstract in AMA style:
Raya-Santos C, Rosas-Gómez de Salazar J, Marco M, Pons-Bas A, Gallego Campuzano R, Cortes J, Pons-Canet L, Shalabi M, Senabre J, Bernal J, Santos-Soler G, Barber X, Garcia Gomez J. Impact of Hydroxychloroquine Level on ECG QTC Interval in Patients with Rheumatic Systemic Autoimmune Diseases: A Real-life Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-hydroxychloroquine-level-on-ecg-qtc-interval-in-patients-with-rheumatic-systemic-autoimmune-diseases-a-real-life-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-hydroxychloroquine-level-on-ecg-qtc-interval-in-patients-with-rheumatic-systemic-autoimmune-diseases-a-real-life-study/