Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Interstitial lung disease (ILD) is a major cause of morbidity and mortality in patients with connective tissue disease (CTD). The aim of our study is to evaluate the impact of hospitalization on clinical outcomes in CTD-ILD patients in a racially and ethnically diverse cohort of patients.
Methods: We queried Clinical Looking Glass (CLG) to conduct a retrospective chart review of patients >18 years of age with radiological or biopsy-proven ILD associated with rheumatologist diagnosed CTD based on ICD9/10 codes who were seen at Montefiore Medical Center between January 2007 and December 2018. Patients who had either 2 CT scans of the chest and/or 2 sets of pulmonary function tests (PFT) at least 6 months apart were included in the study. We collected dataon clinical demographics, cause of hospitalization, length of hospital stay, use of immunosuppression therapy, and mortality. The patients were stratified into 2 cohorts: non-hospitalized and hospitalized. The latter cohort was further sub-stratified into patients with cardiopulmonary vs. non-cardiopulmonary hospitalization (Figure 1). The data were analyzed using Two-sample T-tests orWilcoxon’s rank sum tests for continuous variables, and Chi-square or Fisher’s exact tests for categorical variables as appropriate. Survival analysis was done using the Kaplan-Meier method. Log-rank tests were used to compare differences between the groups. Cox regression models were used to get the hazard ratios with confidence intervals.
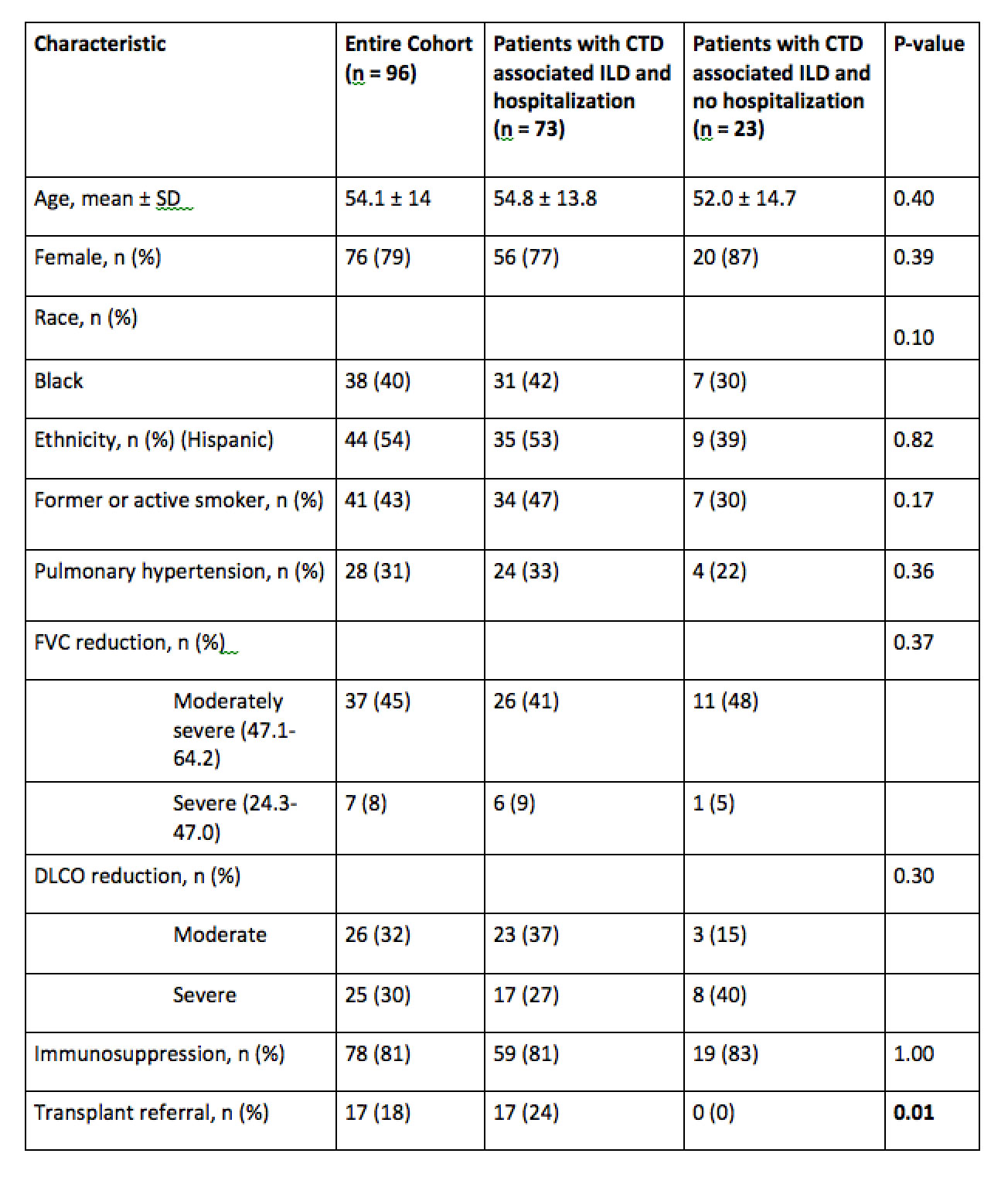
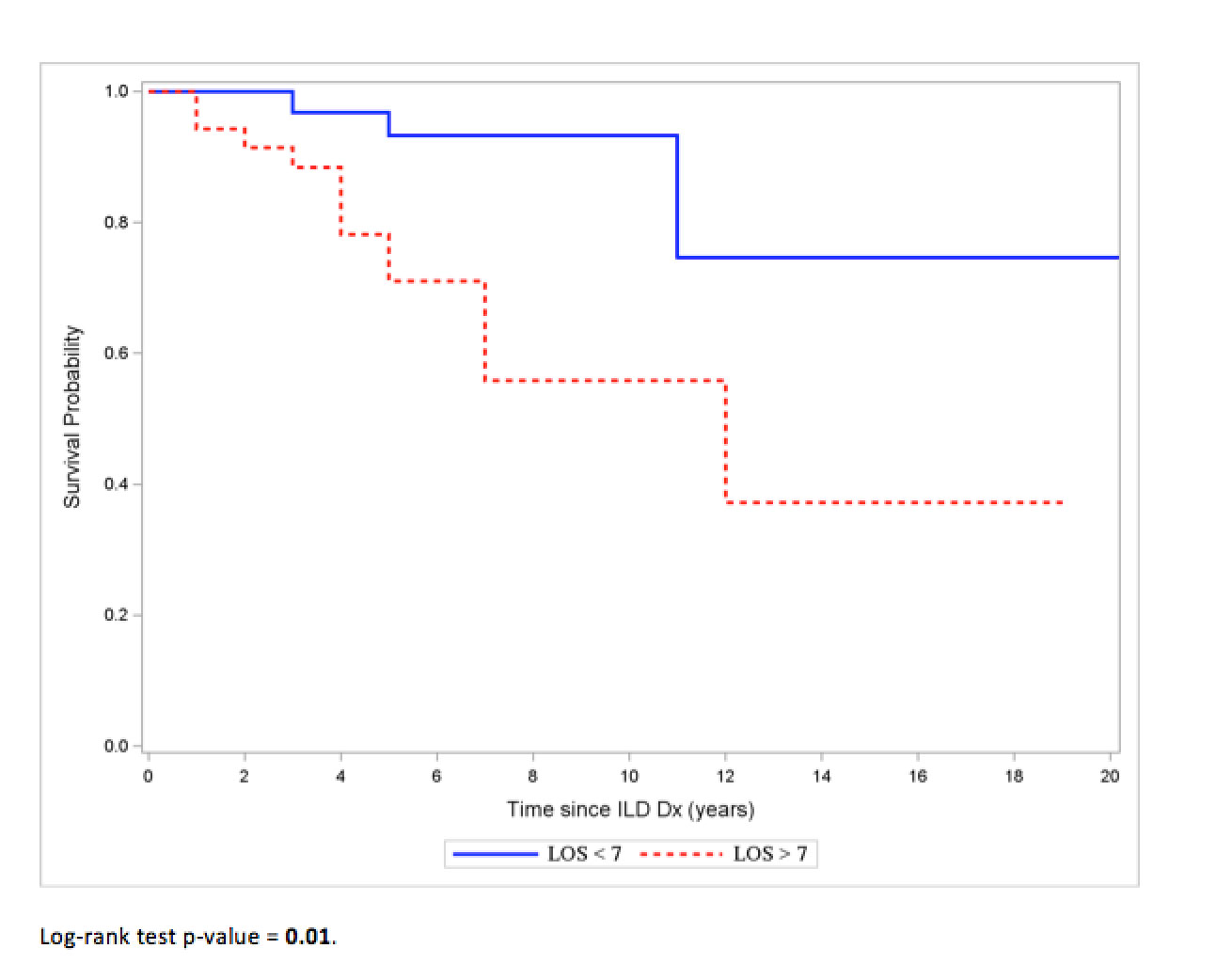
Results: We identified 213 patients with CTD-ILD and 96 met our inclusion criteria (Figure 1). A majority of our patients identified themselves as Black (40%) and Hispanic (54%). The most common CTD was rheumatoid arthritis (29%), followed by inflammatory myositis (22%), and systemic sclerosis (15%). The median duration that the patients had a diagnosis of ILD was 4 years (IQR 5-9 years). Hospitalization was recorded in 73 (76%) patients. Baseline characteristics were similar between the hospitalized and non-hospitalized groups (Table 1). No death was observed in the non-hospitalized group, while the risk of death was significantly higher among the hospitalized group (p-value=0.02). There were 17 patients referred for transplant evaluation and all were from the hospitalized group. When stratified by the cause for hospitalization, 51/73 (70%) had a hospitalization for a cardiopulmonary cause. They were significantly older (Mean+SD) (57.2 +13.1 years) than those admitted with non-cardiopulmonary cause (Mean+SD) (49.2+14.8 years). Older age and length of stay greater than 7 days for cardiopulmonary cause were associated with a higher risk of mortality (HR 1.95, 95% CI: 1.11-3.42, p=0.02; and HR 4.82, 95% CI: 1.37-16.92, p=0.01 respectively) (Figure 2).
Conclusion: In our cohort of patients with CTD-ILD, hospitalization for cardiopulmonary causes, especially with a length of stay exceeding 7 days was associated with increased mortality. This finding can help to identify high-risk patients during hospital admission and arrange close monitoring and multidisciplinary care after discharge.
To cite this abstract in AMA style:
Kaur N, Xie X, Korogodina A, Cleven K, Ayesha B, Kumthekar A. Impact of Hospitalization on Clinical Outcomes in Patients with Connective Tissue Disease-associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/impact-of-hospitalization-on-clinical-outcomes-in-patients-with-connective-tissue-disease-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-hospitalization-on-clinical-outcomes-in-patients-with-connective-tissue-disease-associated-interstitial-lung-disease/