Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Gout is a common disease with effective medical therapies, yet many cases are complicated by providers’ hesitancy to prescribe an adequate dose of urate-lowering therapy (ULT), or patients’ reluctance to take it. In addition, patients with gout often have comorbidities resulting in frequent and complex interactions with the healthcare system. In this study, we sought to investigate the effect of inpatient admission on adherence to allopurinol therapy in patients with gout.
Methods: All hospital admissions to the Salt Lake City (SLC) Veterans Affairs (VA) Health Care System (HCS) between March 2018 and March 2019 involving patients who had an active prescription for allopurinol, and who had been requesting regular refills at the time of hospitalization, were identified. Prevalence of allopurinol prescription rates and adherence to refill requests following discharge were determined, and medical records of patients who had discontinued therapy were reviewed.
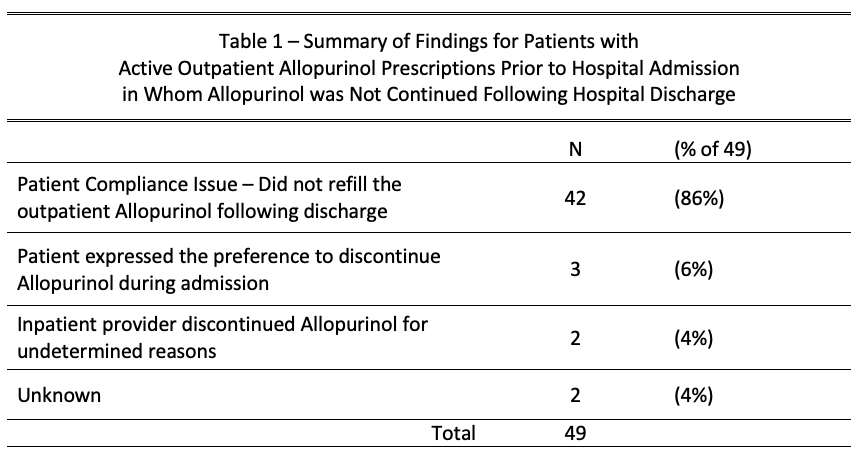
Results: From March 7, 2018 through March 25, 2019, 193 patients with an active prescription of allopurinol were admitted for inpatient care at the SLC VA HCS. These data are summarized in Figure 1. Thirty-one (16%) had not refilled their prescription in the 90 days preceding admission, and were excluded from further analysis. Of the 162 remaining patients, 91 (56%) continued to take allopurinol without change after discharge. The remaining 71 patients did not fill their allopurinol prescription for 90 days after discharge, and were assumed to have stopped taking it. Of these 71 patients, 22 were excluded from the final analysis because they were either taking allopurinol for Tumor Lysis Syndrome (TLS) prophylaxis and no longer needed it (11), were deceased within 90 days of leaving the hospital (7), or filled their prescriptions outside of the VA system (4). Medical records of the remaining 49 patients were reviewed to determine why they stopped taking allopurinol; the findings are summarized in Table 1. In 42 cases (86%), patients did not continue allopurinol despite the inpatient physician recommending they continue it after discharge. The remaining 7 patients had it stopped while inpatient and did not resume it after discharge. The reasons for this were provider recommendation (2), patient preference (3), and unknown (2).
Conclusion: Admission to the hospital is strongly associated with the development of poor adherence to allopurinol therapy in gout patients, even for those who appear to be taking this medication as prescribed before hospitalization. Since patients with gout often have other health problems that require inpatient treatment, this phenomenon may contribute substantially to the major problem of nonadherence to ULT. Additional work is needed to better understand patients’ motivations for stopping treatment, as well as to identify timely and effective interventions in the post-discharge period.
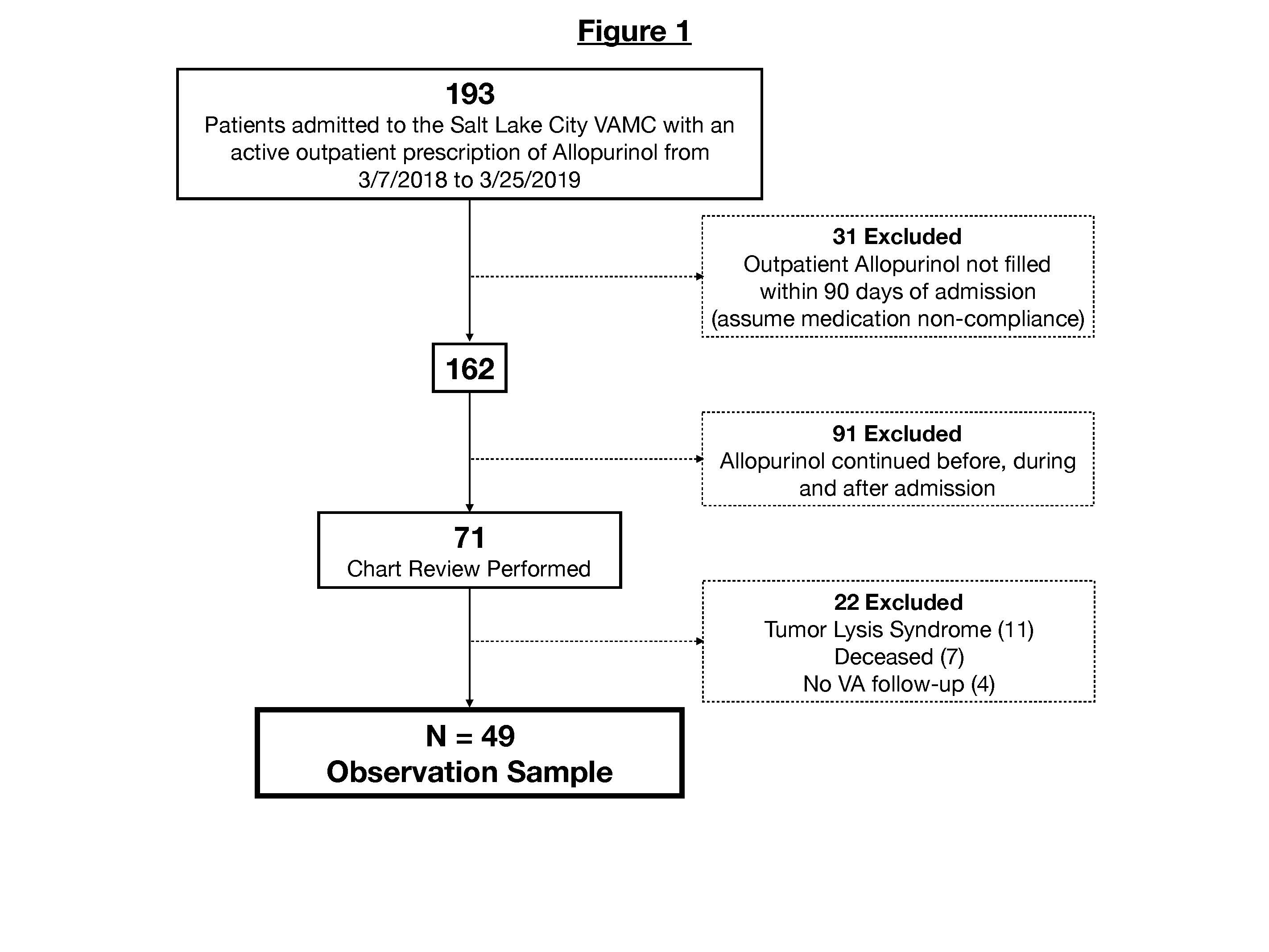
Allopurinol Fig. 1 Admissions Flowchart
To cite this abstract in AMA style:
Lebedoff N, Barker A, Koening C, Jones T, Rose R, Yarbrough P, Battistone M. Impact of Hospital Admissions on Adherence to Allopurinol Therapy After Discharge [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/impact-of-hospital-admissions-on-adherence-to-allopurinol-therapy-after-discharge/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-hospital-admissions-on-adherence-to-allopurinol-therapy-after-discharge/