Session Information
Date: Sunday, October 26, 2025
Title: (0731–0764) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Frailty, a syndrome associated with decreased physiologic reserve, is associated with adverse outcomes. The prevalence and impact of baseline frailty on the risk of mortality in patients with incident giant cell arteritis (GCA) and polymyalgia rheumatica (PMR) is unknown. The objective of this study was to describe the risk of mortality – stratified by frailty – among patients with GCA, PMR, and general population controls.
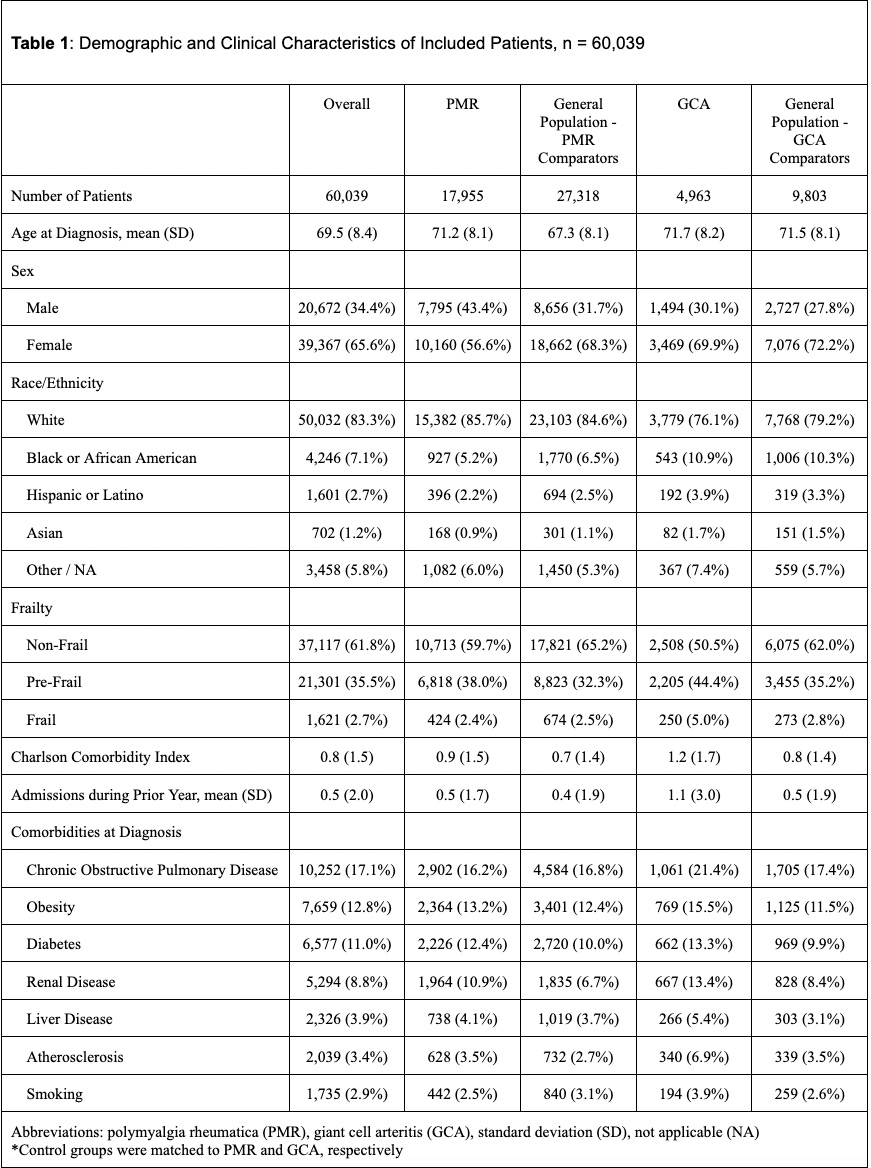
Methods: We conducted a retrospective cohort study using the US-based TriNetX electronic health records network. Adults ≥50 years with new-onset PMR or GCA were included if they had ≥2 ICD-9/10-CM codes, ≥1 year of prior follow-up, and a prednisone prescription within 30 days of the first code (index date). Matched general population control cohorts for PMR and GCA were constructed using 1:3 nearest-neighbor matching on the following variables: sex, race/ethnicity, regional location, birth year, year of cohort entry, and year of cohort exit. The exposure of interest was frailty as measured using a validated claims-based frailty index (CFI) during the year prior to the index date. Multivariable Cox proportional cause-specific hazard ratios (aHR) and 95% confidence intervals (CI) were calculated to assess the risk of mortality.
Results: Of 60,039 included patients, 17,955 had PMR, 4,963 had GCA, and 37,121 were matched controls. Compared to matched general population controls, the risk of death was elevated among patients with GCA (aHR 2.17, 95% CI 1.63-2.90) but not PMR (aHR 0.85, 95% CI 0.71-1.03). In the overall cohort, the risk of death was increased in pre-frail (aHR 2.45, 95% CI 2.03-2.96) and frail (HR 5.16, 95% CI 3.84-6.94) patients as compared to non-frail patients. In the stratified analysis, as compared to non-frail general population controls, the risk of death was not elevated for frail general population controls (aHR 1.27, 95% CI 0.67-2.42) but elevated for non-frail patients with GCA (aHR 1.52, 95% CI 1.20-1.92) and frail patients with GCA (aHR 2.91, 95% CI 1.82-4.66). In a stratified analysis, as compared to non-frail PMR general populations controls, the risk of death was elevated for frail general population controls (aHR 3.04, 95% CI 2.13-4.34) and frail patients with PMR (aHR 1.86, 95% CI 1.17-2.96) but not for patients with PMR who were non-frail (aHR 0.96, 95% CI 0.79-1.15).
Conclusion: Both frailty and GCA were associated with an increased risk of mortality, but patients with PMR did not have an elevated risk of mortality unless they were also frail. Frailty in patients with GCA and PMR identifies a group of patients at risk for mortality and highlights the value of frailty assessment.
To cite this abstract in AMA style:
Hassan F, Putman M, Sattui S. Impact of Frailty on Mortality in GCA and PMR: A Retrospective Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-frailty-on-mortality-in-gca-and-pmr-a-retrospective-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-frailty-on-mortality-in-gca-and-pmr-a-retrospective-cohort/

.jpg)
.jpg)