Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Multiple studies have been done assessing the “weekend effect” and outcomes for hospitalized patients 1,2,3,4, however, there is no data evaluating the outcome of patients with septic arthritis of a native joint (SANJ) who are admitted on the weekend compared to the rest of the week. We evaluated whether important outcomes in SANJ, including in-hospital mortality, differ between patients admitted on weekends versus weekdays and the time to diagnostic arthrocentesis.
Methods: The National Inpatient Sample (NIS) database of the year 2016 was utilized for patients admitted to the hospital with a principal discharge diagnosis of SANJ. This was a retrospective cohort study of patients hospitalized in 2016 with SANJ in hospitals across the US. Patients were included if they were adults with a principal diagnosis of SANJ based on ICD-10 codes. Admissions between midnight Friday and midnight Sunday were classified as weekend admissions. Early arthrocentesis was defined as percutaneous arthrocentesis performed within 24 hours of admission. The proportion of patients with SANJ admitted over weekends versus weekdays was determined. Odds ratios (OR) were calculated for primary and secondary outcomes including in-hospital mortality rate, rates of diagnostic arthrocentesis and early arthrocentesis, length of stay and total hospital charges, These results were compared after multivariable logistic regression adjusted for age, gender, race, day of admission, Charlson comorbidity index and median household yearly income in the patient’s zip code. We used STATA-15 for statistical analysis.
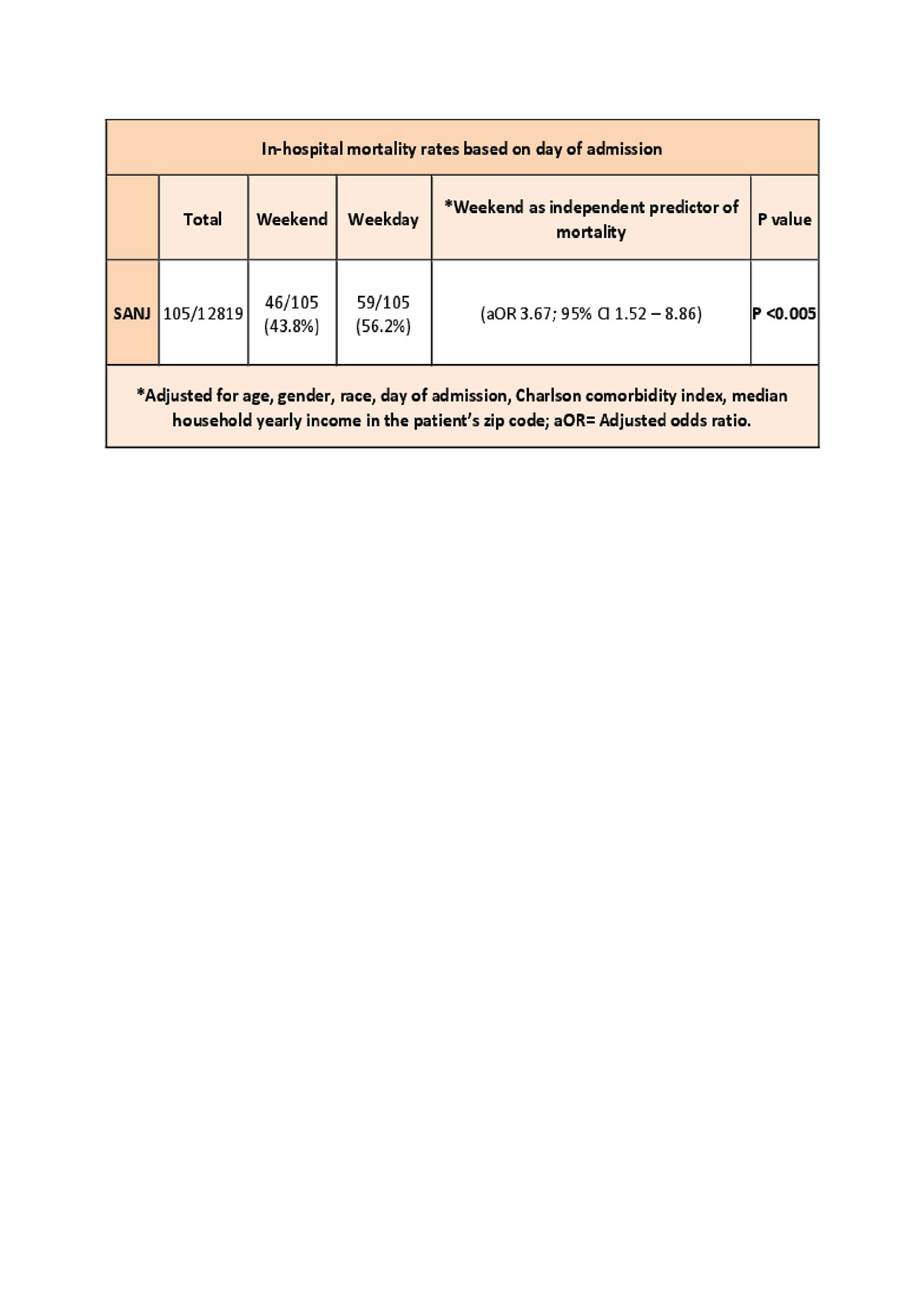
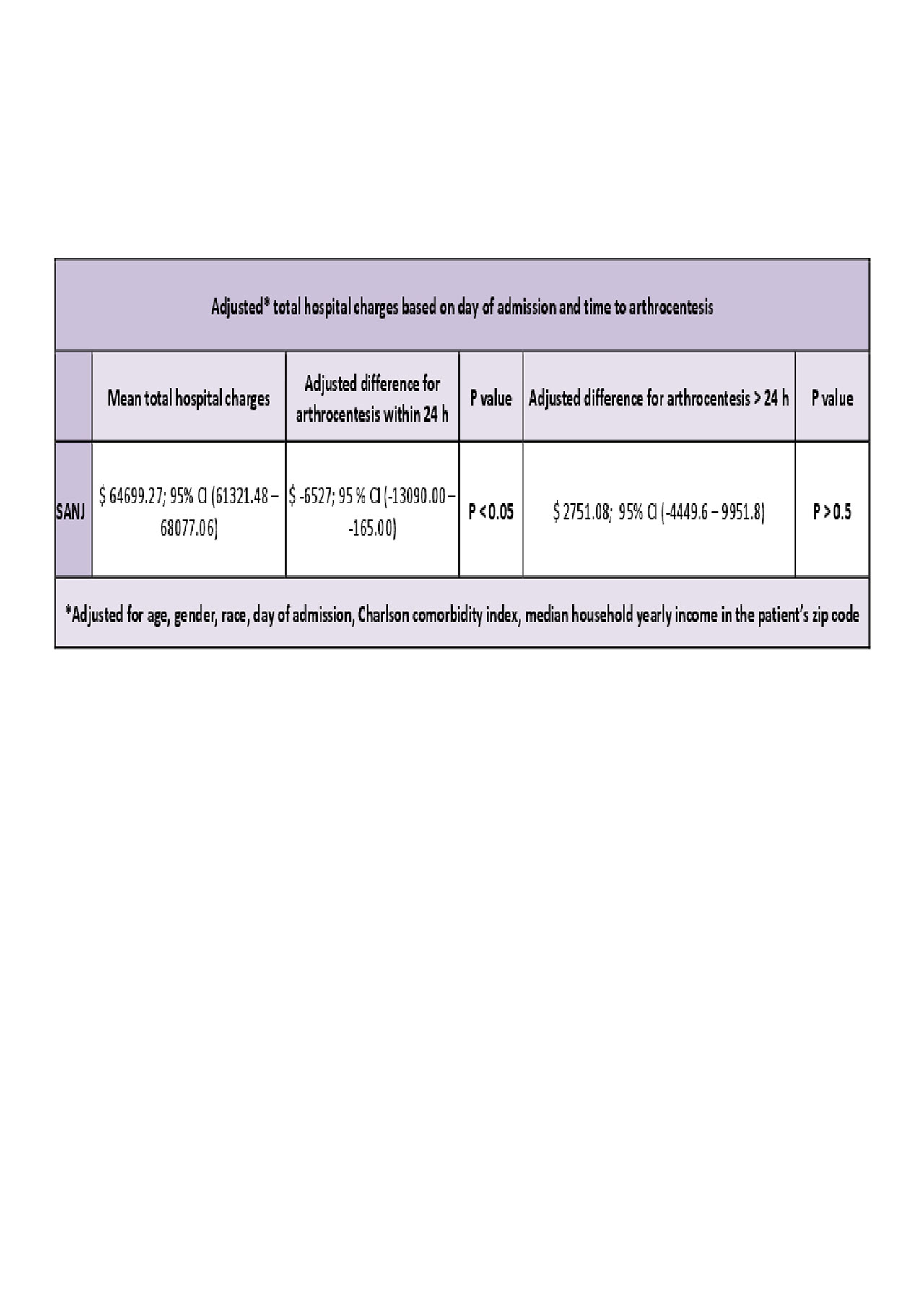
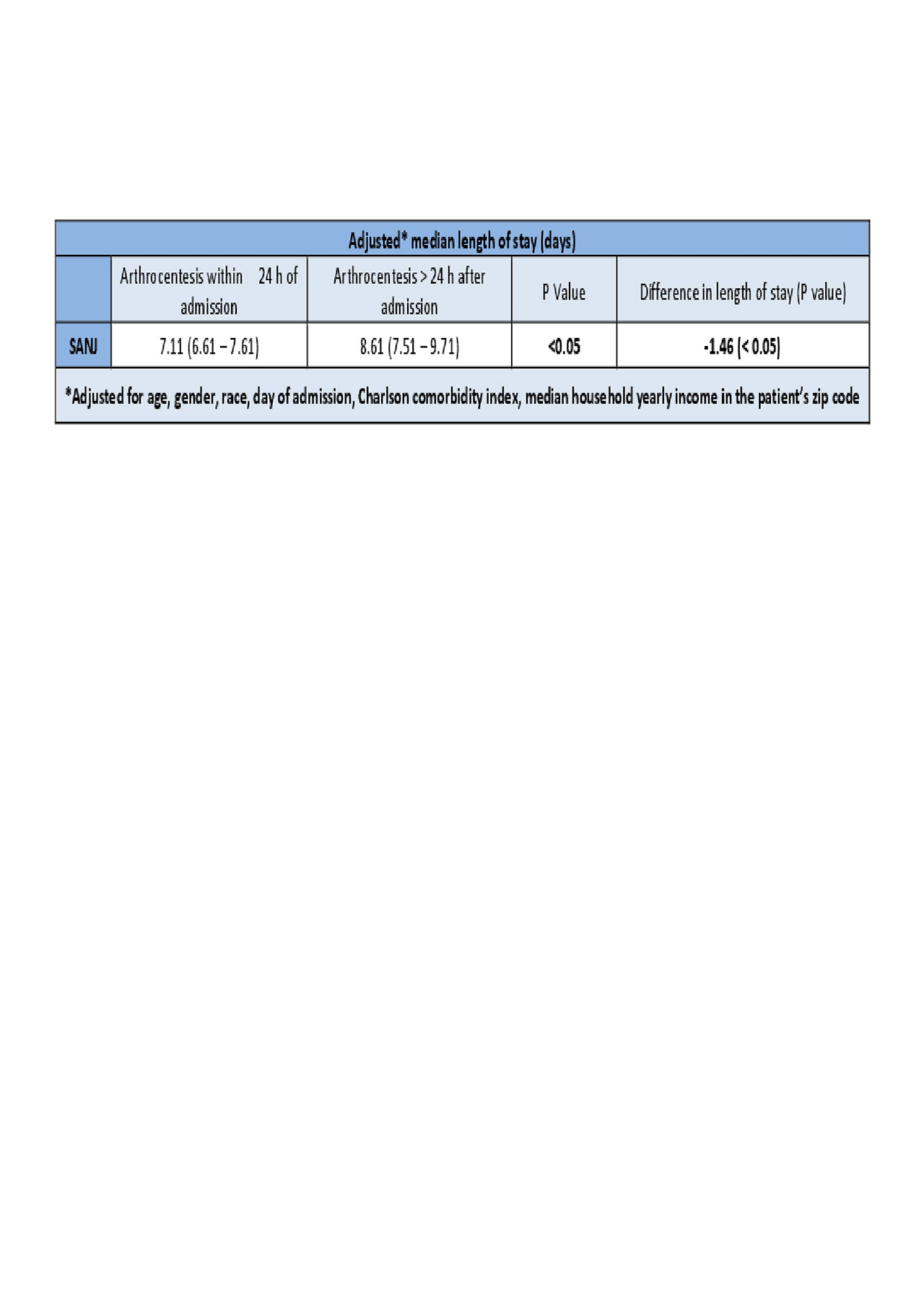
Results: The study included 12819 patients with SANJ. Compared with patients admitted on weekdays, patients with SANJ admitted on weekends had increased in-hospital mortality rates (adjusted odds ratio[aOR] 3.67; 95% [CI] 1.52 – 8.86, p< .005), but similar early arthrocentesis rates ([aOR] 1.14; 95%, [CI] 0.90 – 1.45 p >0.05), length of stay (p >0.05) and hospital charges ($ 2751.11; 95% [CI] -4449.6 – 9951.8; P >0.05). However, regardless of the day of admission those who received an early arthrocentesis had lower length of stay (-1.46, p< 0.05), and lower total hospital charges ($ -6527 $; p< 0.05).
Conclusion: This study showed that compared with patients admitted on weekdays, patients with SANJ admitted on weekends had increased mortality rates but similar length of stays and total hospital charges. However, patients who received an early arthrocentesis had significantly lower length of stay and hospital charges regardless of the day of admission. This results add weight to the hypothesis of negative outcomes in weekend admissions. Moreover, we believe that our findings require further investigation to establish the role of early arthrocentesis in the management of septic arthritis.
To cite this abstract in AMA style:
Contreras G, Arevalo A, Murray S, Haddadin F, Luo Y. Impact of Day of Admission and Time to Diagnostic Arthrocentesis on Mortality and Other Outcomes in Septic Arthritis: A Nationwide Analysis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/impact-of-day-of-admission-and-time-to-diagnostic-arthrocentesis-on-mortality-and-other-outcomes-in-septic-arthritis-a-nationwide-analysis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-day-of-admission-and-time-to-diagnostic-arthrocentesis-on-mortality-and-other-outcomes-in-septic-arthritis-a-nationwide-analysis/