Session Information
Date: Tuesday, November 14, 2023
Title: (2019–2038) Patient Outcomes, Preferences, & Attitudes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The COVID-19 pandemic created significant barriers to accessing recommended preventative health screening. Patients already managing a chronic disease, particularly those using immunosuppressive medications, may have been disproportionately impacted due to heightened concerns about nosocomial COVID-19 infection risks. The goal of this study was to identify delays in preventative health screening among rheumatology outpatients and assess risk factors associated with delays.
Methods: Between 03/09/2022 and 06/15/2022, 9918 adults enrolled in a single center COVID-19 Rheumatology Registry in New York City were asked whether they skipped or delayed pap smears, mammograms and/or colonoscopy screenings due to the COVID-19 pandemic. Participants living in NY, NJ, or CT were also assigned a census tract-based Social Vulnerability Index (SVI). ICD-10 algorithms identified systemic rheumatic diseases (SRDs). We compared differences between those who did or did not delay screenings using Chi-square, Fisher’s exact, or Wilcoxon rank-sum tests as appropriate. We used multivariable models to assess risk factors associated with delay of each screening test in both the whole cohort and separately in the subgroup with SVI scores.
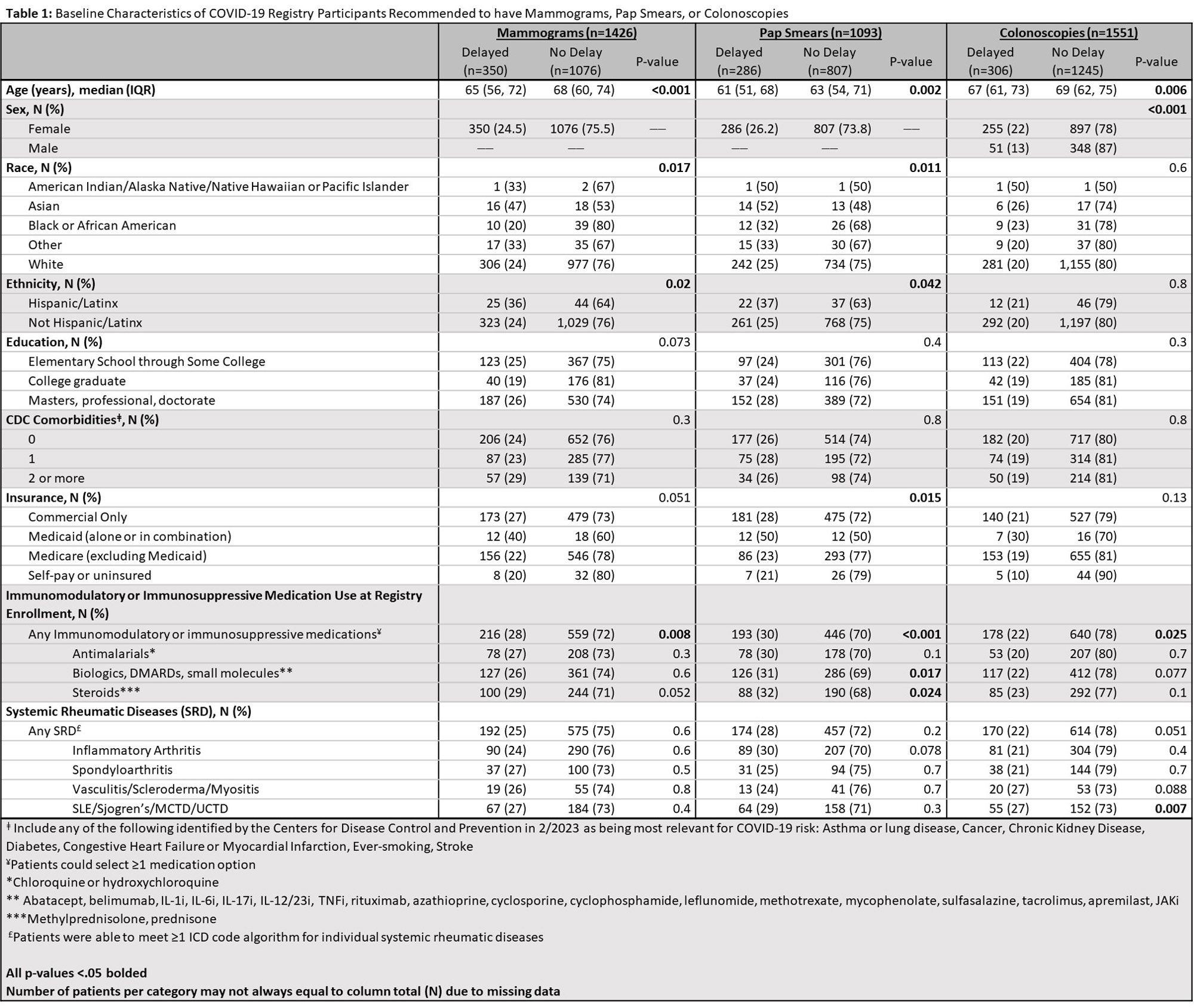
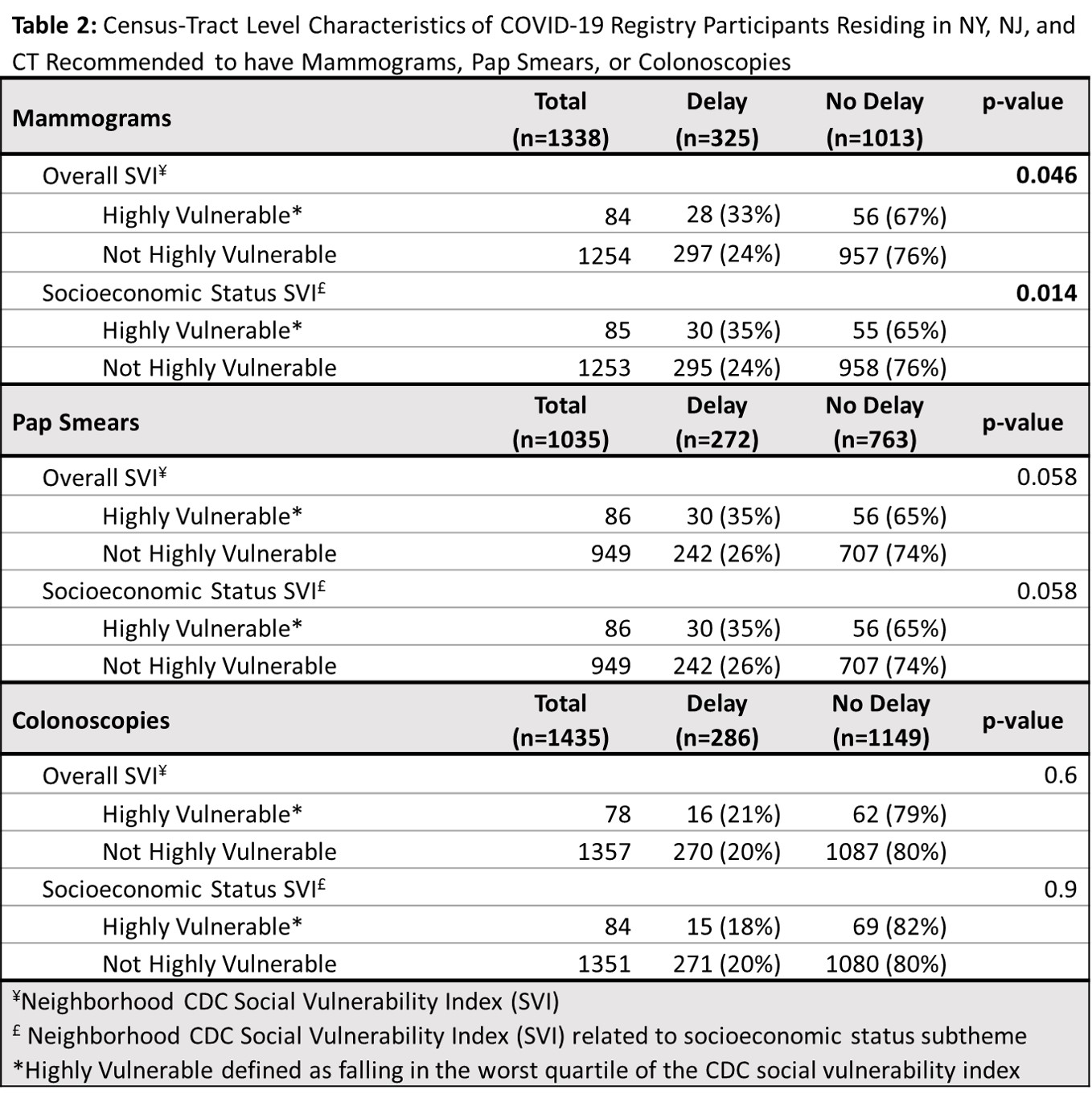
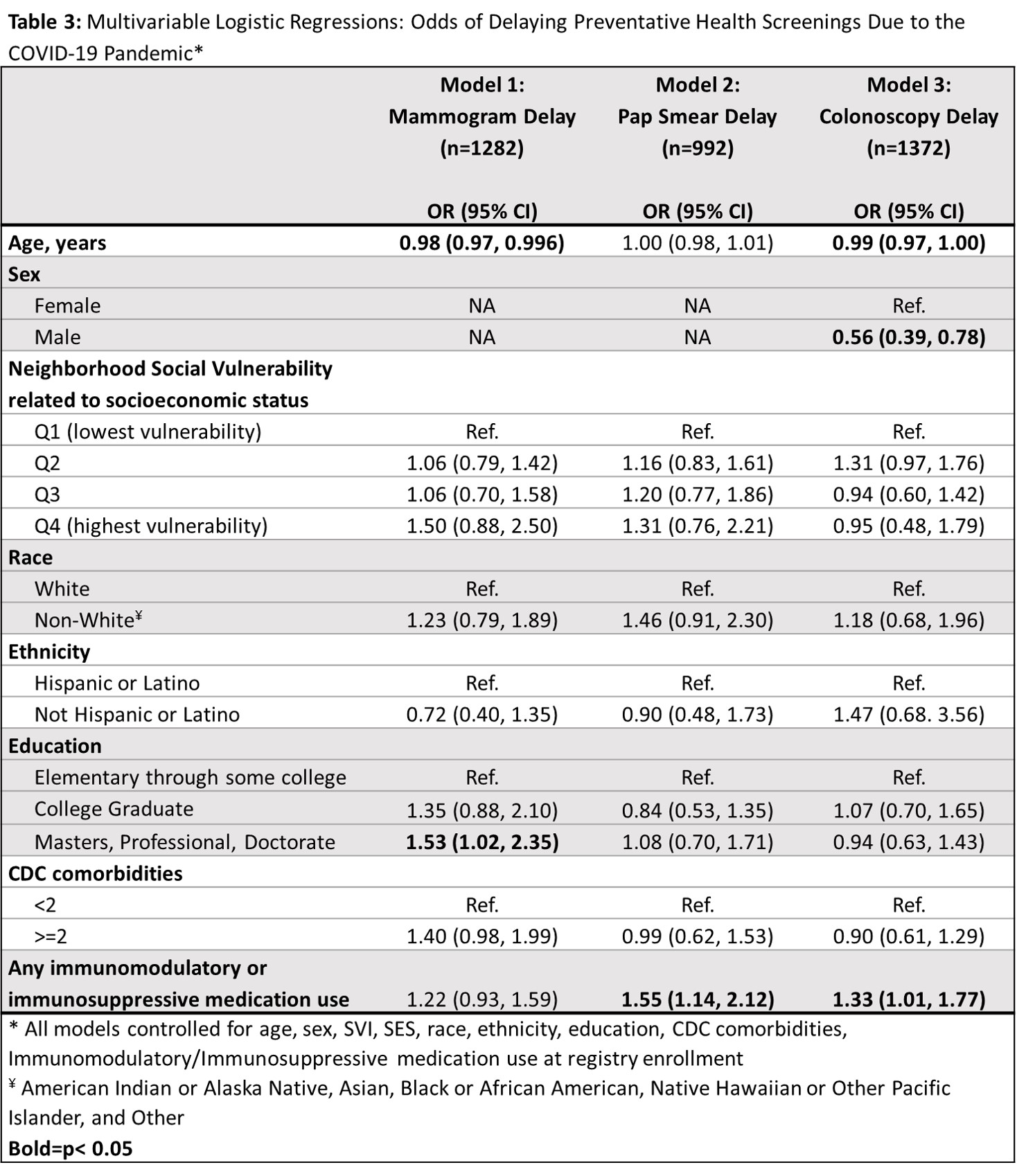
Results: 2735/9918 (27.6%) participants responded. Mean age was 65.4 years (SD=12.7), 90.6% White, 4.6% Hispanic/LatinX. 2000 were recommended to have regular preventive health screens. Delays were reported in 286/1093 pap smears (26.2%); 350/1426 mammograms (24.5%); and 306/1551 colonoscopies (19.7%). More Hispanic/LatinX vs. non-Hispanic/LatinX participants delayed pap smears (37% vs. 25%, p=.04) and mammograms (36% vs. 24%, p=.02). Fewer White participants delayed pap smears (25% of White participants delayed, 32% Black, 52% Asian, 33% Other; p=.01). Mammogram delays also differed by race (24% of White participants delayed, 20% Black, 47% Asian, and 33% Other; p=.02). More females than males delayed colonoscopies (22% vs. 13%, p < .001). Younger age was associated with delaying all three screens (all p< 0.05). Participants living in census tracts with the worst socioeconomic vulnerability had higher proportions of delayed mammograms (35% vs. 24%, p=.01). Participants using any immunomodulatory/immunosuppressive medication at registry enrollment were more likely to report delaying all three screens (p=.03). Having an SRD was not associated with delays. In multivariable models, adjusting for all other covariates, those on immunomodulatory/immunosuppressive medications were more likely to delay pap smears (OR 1.55, 95% CI: 1.14, 2.12) and colonoscopies (OR 1.33, 95% CI: 1.01, 1.77), but not mammograms (OR 1.22, 95% CI: 0.93-1.59). Males were less likely to delay colonoscopies (OR 0.55, 95% CI: 0.39, 0.78). For every one-year increase in age, the odds of delaying a mammogram decrease by 1.7% (OR 0.98, 95% CI: 0.97, 0.996).
Conclusion: Immunomodulatory/immunosuppressive medications but not SRD diagnosis was associated with preventive screening delays. These data can help identify rheumatology patients at risk for preventative screening delays. The impact of race, ethnicity, and SES on delaying health screening should be explored in more diverse populations.
To cite this abstract in AMA style:
Nong M, Barbhaiya M, Levine J, Bykerk V, Heise R, Mandl L. Impact of COVID-19 Pandemic on Preventative Health Screenings in Rheumatology Outpatients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/impact-of-covid-19-pandemic-on-preventative-health-screenings-in-rheumatology-outpatients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-covid-19-pandemic-on-preventative-health-screenings-in-rheumatology-outpatients/