Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: SLE patients are prone to hospitalizations and readmissions compared to general population. Depression is highly prevalent among patients with SLE and is an important inpatient comorbidity. Studies have established that depression is an independent risk factor for CVD and premature CVDs are a major cause of mortality in SLE. The additive effect of depression on CVD in SLE remains unknown. Hence, we aimed to investigate the impact of co-morbid depression on SLE hospitalizations in terms of mortality or CVD outcomes and readmissions.
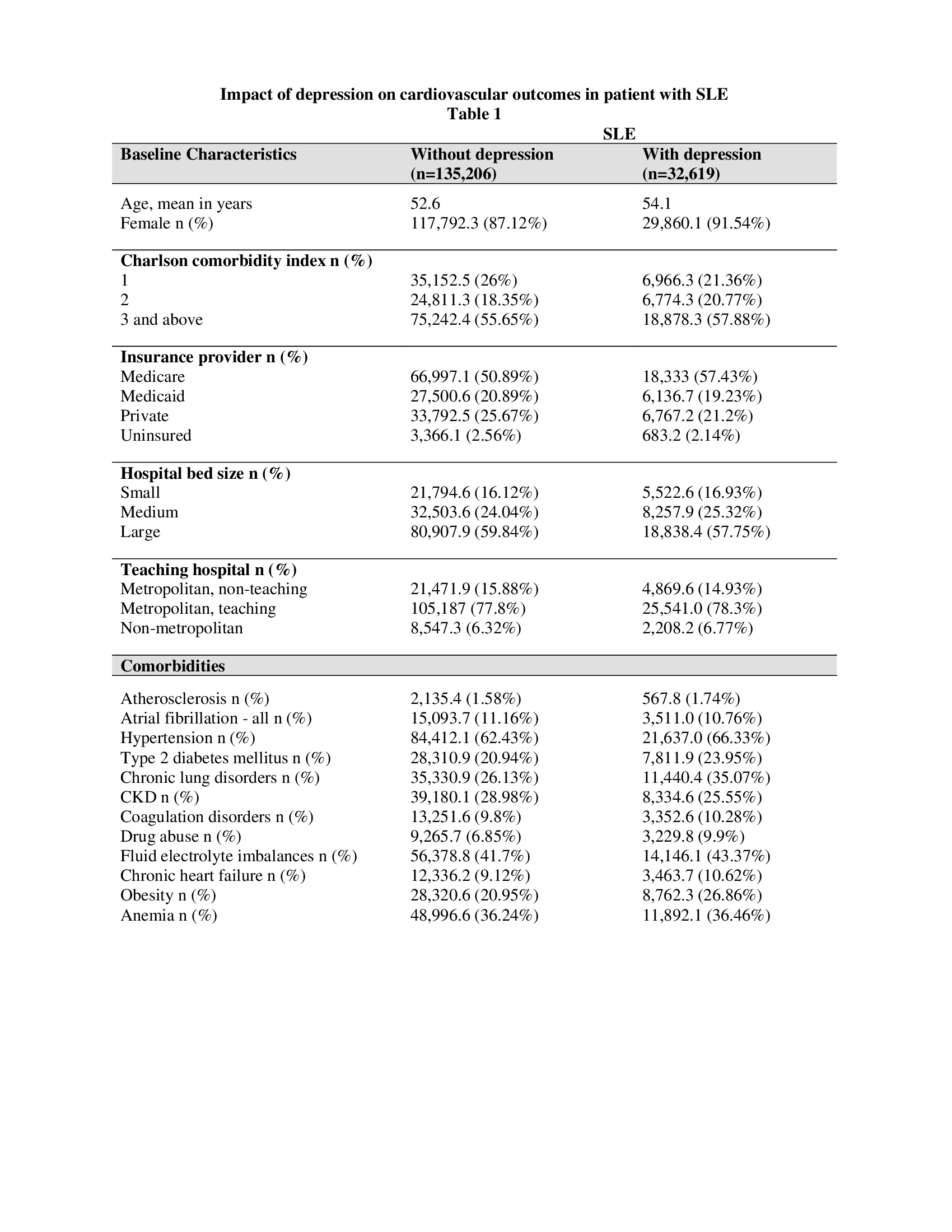
Methods: We performed a retrospective analysis using the 2020 National readmission database (NRD) and identified patients over 18 years of age hospitalized with a principal diagnosis of SLE (ICD 10 code: M32). NRD is a nationally representative database that has discharge data from 31 states and weighted, estimates over 32 million discharges in a year. Depression was identified using ICD 10 codes (F32, F33, F34.1) and SLE patients were divided into two subgroups based on presence or absence of co-morbid depression. Baseline characteristics including demographics, hospital level variables and co-morbidities (table 1) were identified for the two groups. Nearest propensity matching (PSM) was performed using a 1:1 ratio for all baseline characteristics. The primary outcome of interest was mortality. Secondary outcomes include ischemic stroke, acute myocardial infarction, acute heart failure, vasopressor use, acute kidney injury, 30- and 90-day readmissions. T-test and chi-square tests were performed to compare outcomes and p value < 0.05 was considered statistically significant. STATA 18 was used to perform the analysis.
Results: Among 167,825 SLE hospitalizations, 32,619 (19.4%) had co-morbid depression. Baseline characteristics are shown in Table 1. After matching, SLE patients with depression have low all-cause mortality rates (2.05% vs 2.98%, p < 0.001). No significant impact seen on 30- and 90- day readmission rates (8.26% vs 8.09%, p 0.581, and 7.03% vs 6.73%, p 0.267 respectively), and incidence of ischemic stroke (2.00 vs 2.26%, p < 0.100). However, depression reduced acute MI (5.14% vs 6.34%, p< 0.001), acute HF (7.16 vs 7.88%, p 0.012), vasopressor use (0.68% vs 0.93%, p 0.009), and AKI (19.71% vs 21.27%, p < 0.001) (Table 2).
Conclusion: Depression was highly prevalent among hospitalized SLE patients and traditional CVD risk factors such as DM, HTN, and obesity were noted to be higher in the SLE + depression group. However, co-morbid depression did not impact readmissions, or adverse cardiovascular events. Interestingly, a significant reduction in all- cause mortality was seen. Further studies are warranted to analyze the reasons for hospitalizations and readmission in this subgroup which may help providers predict morbidity and mortality and provide tailored medical care.
To cite this abstract in AMA style:
Gandhi S, Challa A, Kanniyaram S, Kamat A, Polana T, Michaud K. Impact of Co-morbid Depression on Systemic Lupus Erythematosus Hospitalizations: Insights from National Readmission Database 2020 [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/impact-of-co-morbid-depression-on-systemic-lupus-erythematosus-hospitalizations-insights-from-national-readmission-database-2020/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-co-morbid-depression-on-systemic-lupus-erythematosus-hospitalizations-insights-from-national-readmission-database-2020/