Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Proteinuria is a marker of lupus nephritis (LN) activity, damage, and response to therapy. There is still sparse evidence on the renal outcomes associated with low-level proteinuria (≤1 g/day). In this study, we aimed to explore the impact of baseline proteinuria levels on renal outcomes.
Methods: We included 249 patients diagnosed with their first biopsy-proven LN. We divided patients based on baseline proteinuria into low-level (≤1 g/day, group 1; 62 patients), moderate-level ( >1 and < 3 g/day, group 2; 90 patients), and high-level proteinuria (≥3 g/day, group 3; 97 patients). Outcomes included: 1- Complete proteinuria recovery (CPR) (< 0.5 g/day) at 1 year, 2- An adverse composite outcome of end-stage kidney disease (estimated glomerular filtration rate [eGFR] < 15 mL/min/1.73 m2, dialysis, or kidney transplant), a sustained ≥40% decline in eGFR, or death, and 3- LN flares, defined as doubling of proteinuria to ≥1 g/day after complete response or to ≥2 g/day after partial response. Univariable and multivariable Cox proportional hazard models were used to examine the association between baseline characteristics and long-term outcomes.
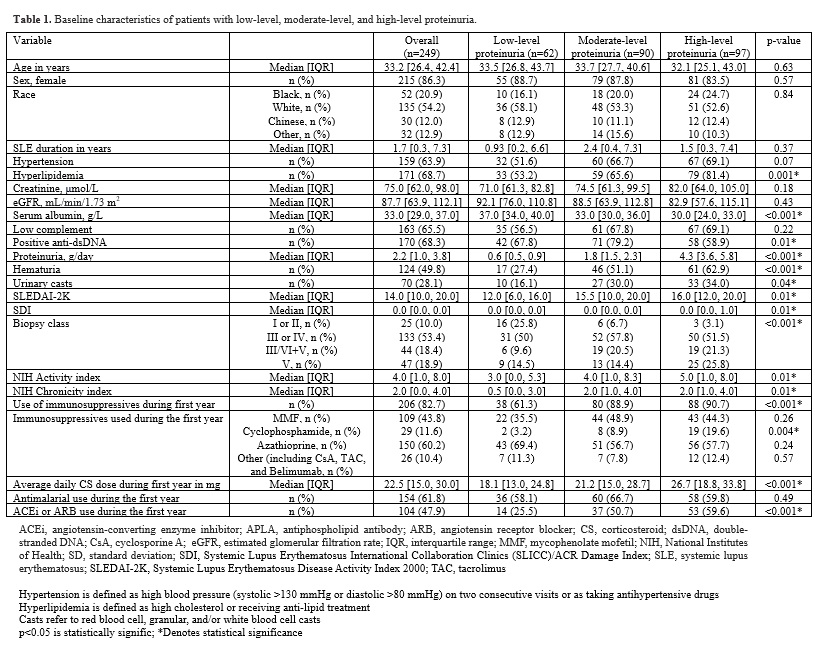
Results: At baseline, the median [IQR] age of our cohort of 249 patients was 33.2 [26.4, 42.4] years; median proteinuria level was 2.2 [1.0, 3.8] g/day. 177 (71.1%) patients had proliferative LN; 59.7% in group 1, 78.9% in group 2, and 71.4% in group 3. There were significant differences between the three groups in baseline disease-related characteristics (Table 1), with a trend of severity concordant with the proteinuria level (worst for group 3).
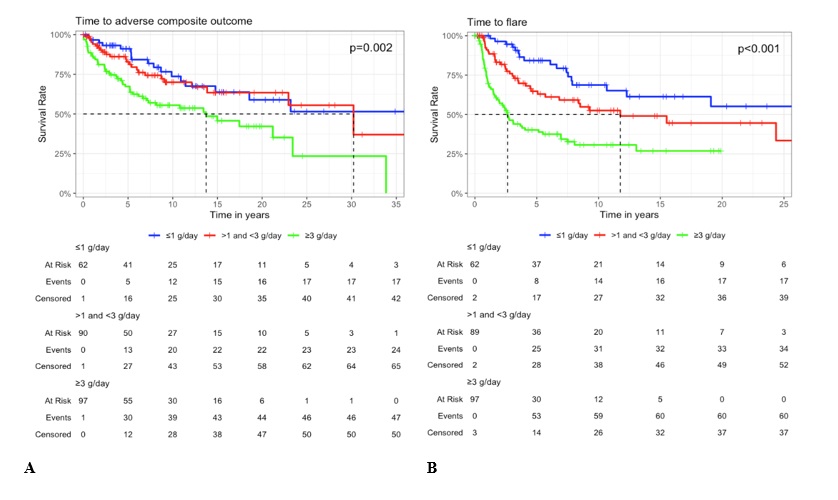
The rate of achievement of CPR at 1 year was highest for group 1 and lowest for group 3; 58.7% (group 1), 41.1% (group 2), and 38.1% (group 3). For long-term outcomes (median follow-up 8.4 years), the frequency of the adverse composite outcome was 27.4%, 26.7%, and 48.5% in groups 1, 2, and 3, respectively; p=0.003. The corresponding frequency of flares was 27.4%, 38.2%, and 61.9%, respectively; p< 0.001. Kaplan-Meier curves showed a shorter time to the adverse composite outcome and LN flares in group 3 compared to groups 1 and 2 (Figure 1).
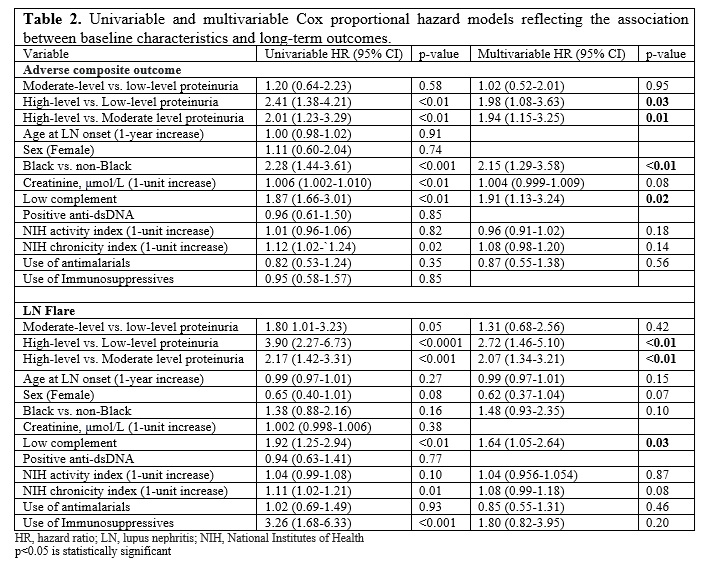
In the multivariable model (Table 2), group 3 was significantly associated with developing the adverse composite outcome and LN flares compared to groups 1 and 2; the risk of developing both outcomes was comparable between groups 1 and 2. Factors significantly associated with the adverse composite outcome included: high-level vs. low-level proteinuria (HR 1.98, p=0.03), high-level vs. moderate-level proteinuria (HR 1.94, p=0.01), Black vs. non-Black race (HR 2.15, p< 0.01), and hypocomplementemia (HR 1.91, p=0.02). Factors significantly associated with LN flares included: high-level vs. low-level proteinuria (HR 2.72, p< 0.01), high-level vs. moderate-level proteinuria (HR 2.07, p< 0.01), and hypocomplementemia (HR 1.64, p=0.03).
Conclusion: LN presenting with low-level proteinuria is commonly associated with proliferative disease, kidney function decline, and renal flares. The risk of developing adverse renal outcomes is comparable between patients with low and medium-level proteinuria at baseline but greatest with high-level proteinuria.
A- Time to adverse composite outcome (end-stage kidney disease, a sustained ≥40% decline in eGFR, or death)
B- Lupus nephritis flare
To cite this abstract in AMA style:
Kharouf F, Li Q, Whittall Garcia L, Gladman D, Touma Z. Impact of Baseline Proteinuria Level on Long-term Outcomes in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-baseline-proteinuria-level-on-long-term-outcomes-in-lupus-nephritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-baseline-proteinuria-level-on-long-term-outcomes-in-lupus-nephritis/