Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Antiphospholipid syndrome (APS) is recognized for its association with an elevated risk of ischemic strokes and other thromboembolic events. This study aims to compare the epidemiology and hospitalization outcomes of ischemic stroke patients with and without a secondary diagnosis of APS using a nationwide inpatient database.
Methods: Patients who were 18 or older, and were hospitalized between January 1, 2020, and
December 31, 2020, with a primary diagnosis of ischemic stroke with and without a secondary diagnosis of antiphospholipid syndrome (APS), were identified from the National Inpatient Sample (NIS) database using the International Classification of Diseases, Tenth Revision (ICD-10) codes. The NIS is the largest publicly available all-payer inpatient care database in the United States. The primary outcome was inpatient mortality, and the secondary outcomes were the length of stay (LOS) and the total hospital charge. The odds ratio was calculated using logistic multivariate regression analysis to adjust for age, race, gender, Charlson comorbidity index, and several high-risk comorbidities.
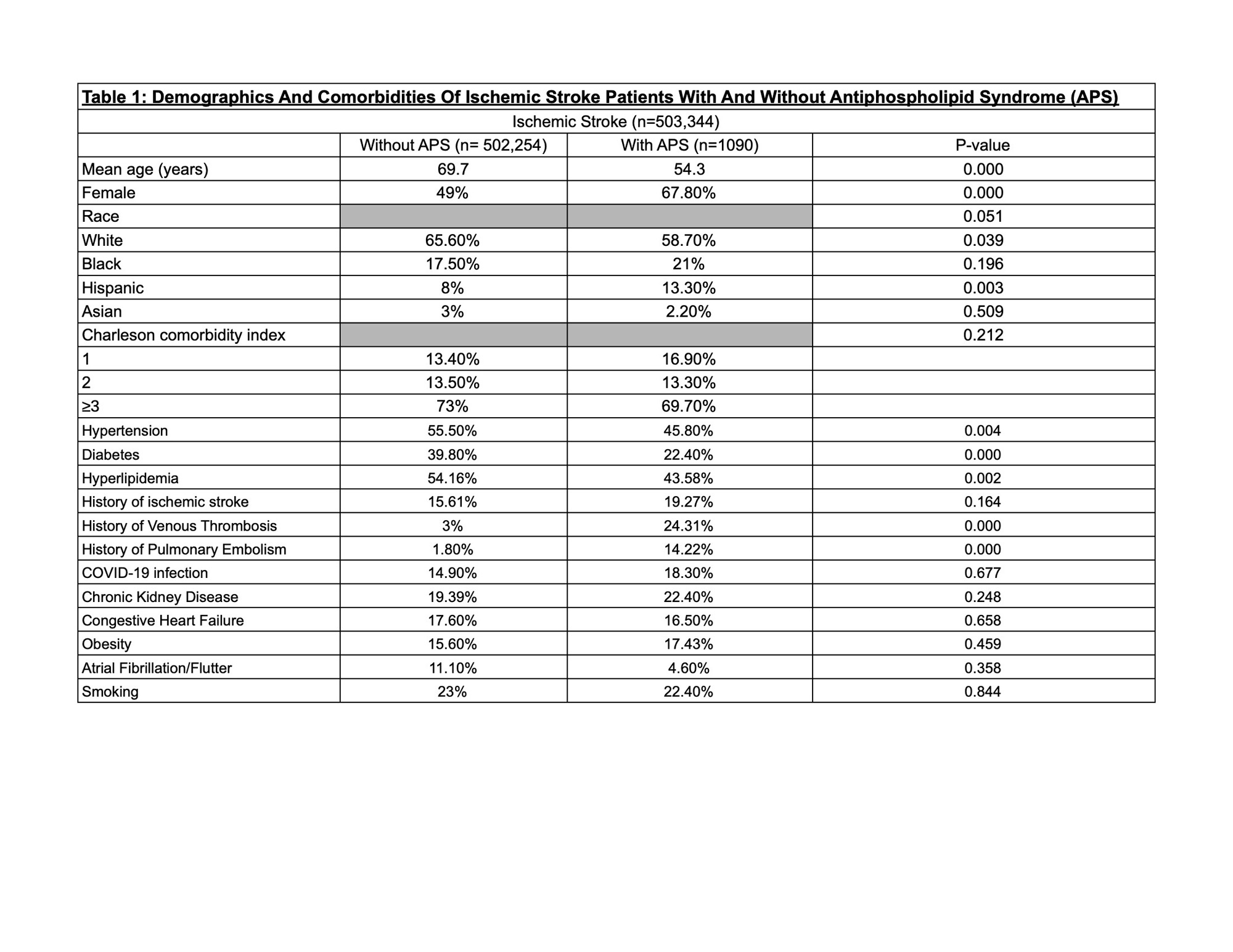
Results: Out of 503,344 patients admitted with a primary diagnosis of ischemic stroke, 1090 (0.21%) had APS. Ischemic stroke patients with APS were younger (54.3 vs 69.7; p=0.000), had more females (67.8% vs 49%; p=0.000), and had a higher prevalence of prior history of pulmonary embolism (14.22% vs 1.8%; p=0.000), and venous thrombosis (24.31% vs 3%; p=0.000) compared to stroke patients without APS. The APS group had a lower prevalence of diabetes (22.4% vs 39.8%; p=0.000), hypertension (45.8% vs 55.5%; p=0.004), and hyperlipidemia (43.58% vs 54.16 %; p=0.002) compared to Ischemic stroke patients without APS. Other differences in demographic and comorbidity trends were insignificant between both groups.
Demographics and prevalence of comorbidities are summarized in Table 1.
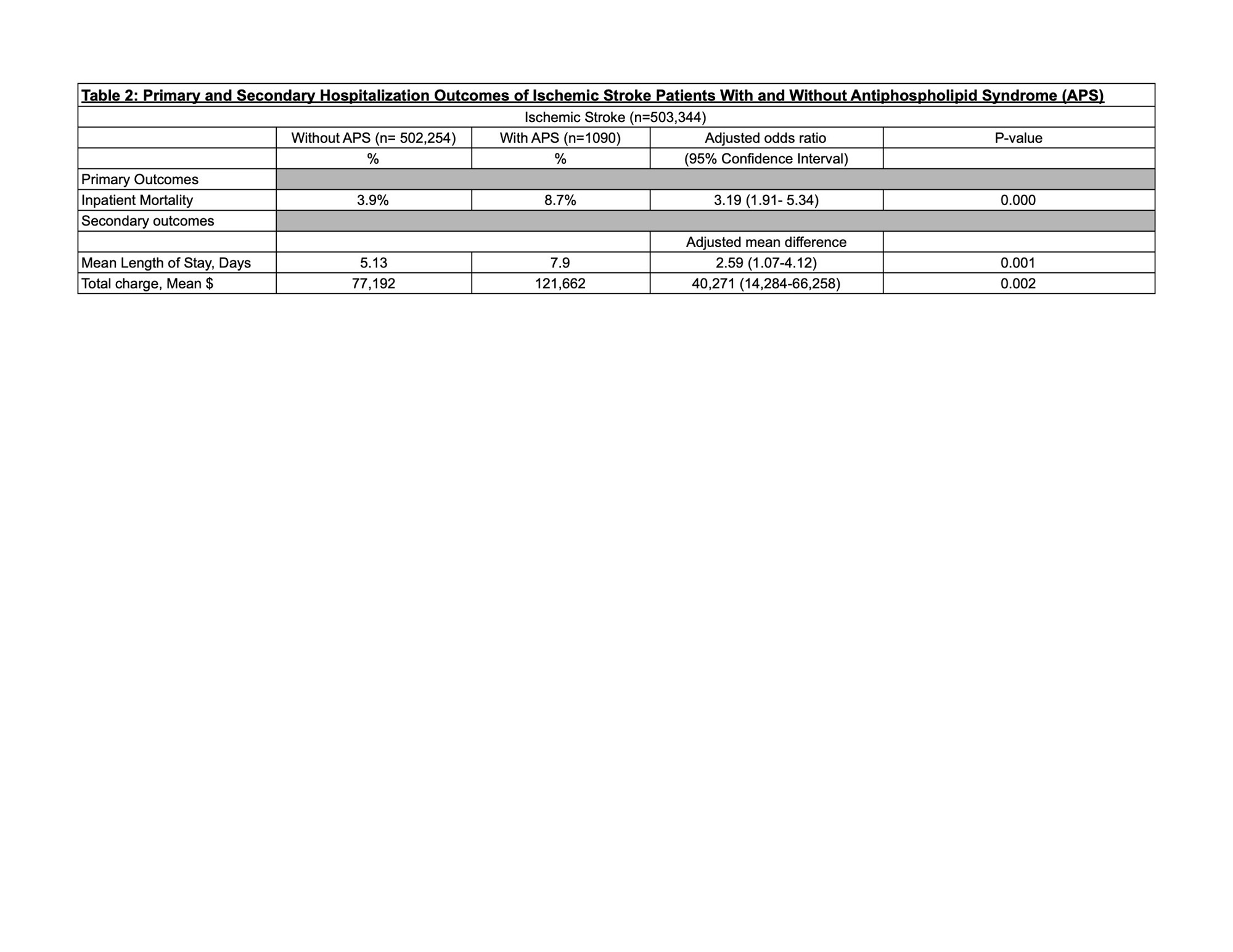
Ischemic stroke hospitalizations with APS were significantly associated with higher inpatient mortality (adjusted odds ratio [AOR] 3.19; 95% Confidence Interval [CI] 1.91- 5.34; p=0.000),
longer mean length of stay (2.59 more days; CI 1.05-4.12; p=0.001), and higher total hospital charges ($121,662 vs $77,192; CI $14,284-$66,258; p=0.002) compared to ischemic stroke patients without APS.
Primary and secondary hospitalization outcomes are summarized in Table 2.
Conclusion: Patients hospitalized with ischemic stroke and APS had higher inpatient mortality rates, longer hospital stays, and incurred greater hospital charges compared to ischemic stroke patients without APS.
To cite this abstract in AMA style:
Rabah S. Impact of Antiphospholipid Syndrome on Mortality of Hospitalized Ischemic Stroke Patients: A Retrospective Analysis of the National Inpatient Sample Database 2020 [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/impact-of-antiphospholipid-syndrome-on-mortality-of-hospitalized-ischemic-stroke-patients-a-retrospective-analysis-of-the-national-inpatient-sample-database-2020/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-antiphospholipid-syndrome-on-mortality-of-hospitalized-ischemic-stroke-patients-a-retrospective-analysis-of-the-national-inpatient-sample-database-2020/