Session Information
Date: Tuesday, November 14, 2023
Title: (2370–2386) Vasculitis – ANCA-Associated Poster III: Biomarkers & Renal Outcomes
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The aim of this study was to investigate the relationship between ANCA specificity and the risk of major adverse cardiovascular events (MACE) in patients with ANCA-associated vasculitis (AAV).
Methods: We conducted a retrospective study using the ANCA-associated vasculitis Toulouse cohort (AAVT). The incidence of MACE, defined as myocardial infarction (MI) and/or stroke and/or death, as well as survival, were compared among patients according to their ANCA specificity. We also applied Cox regression models adjusted for traditional cardiovascular risk factors and sex to assess the risk of MI, stroke and MACE occurrence.
Results: A total of 402 patients were included, of whom 166 (41%) had anti-PR3 ANCA and 236 (59%) had anti-MPO ANCA. Among them, 220 (55%) were male and 182 (45%) were female. The mean age at diagnosis was 61.22 (SD: 16.05) years, and the mean follow-up duration was 7.51 (SD: 6.41) years. During the study period, 15 cases of MI and 12 cases of stroke were identified.
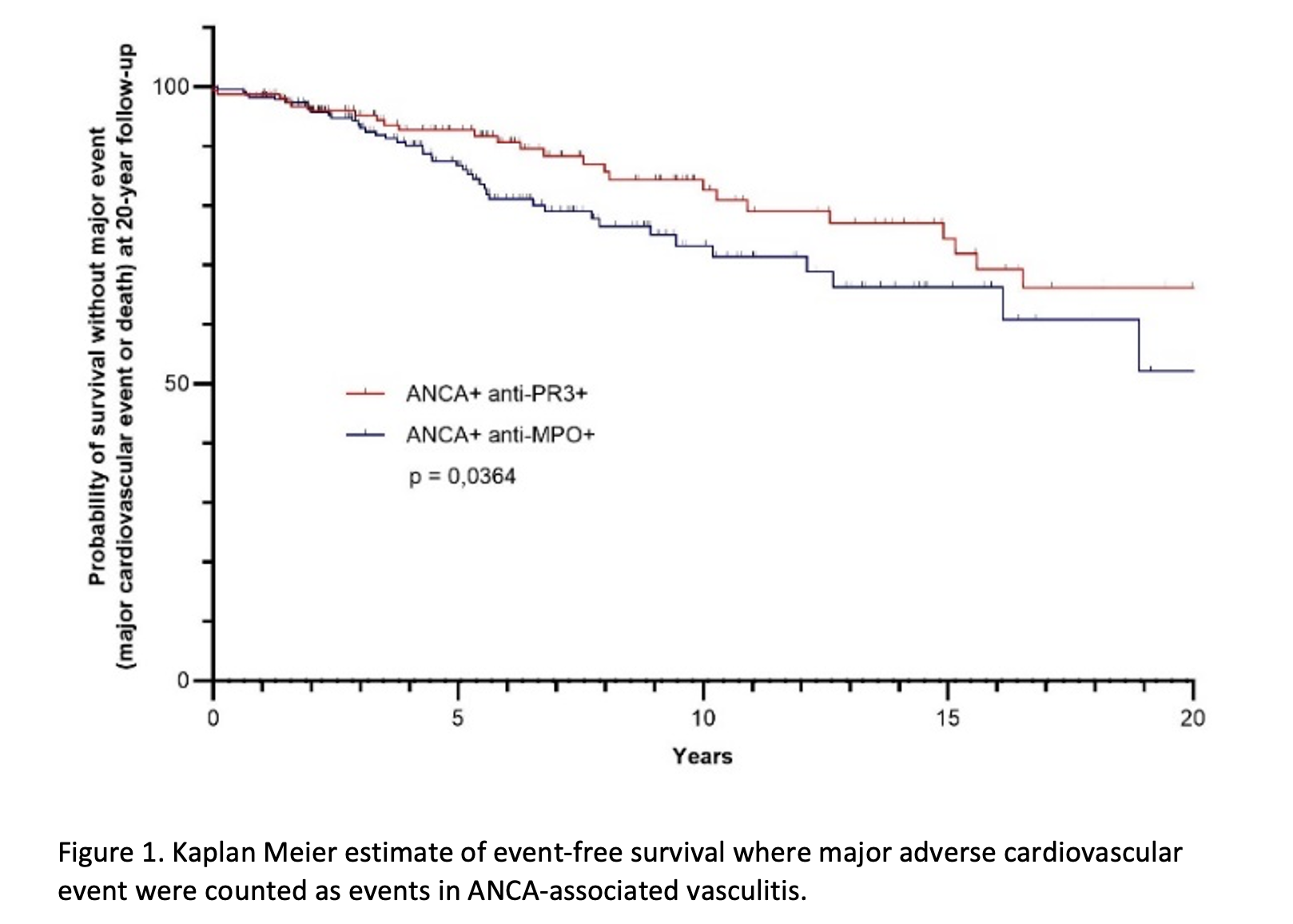
The incidence rate of MACE was 33.11 per 1000 patient-years in the anti-MPO ANCA group, compared to 21.37 per 1000 patient-years in the anti-PR3 ANCA group. The mean time to MACE occurrence was 3.29 (SD: 2.74) years in the anti-MPO ANCA group and 7.33 (SD: 5.68) years in the anti-PR3 ANCA group (p=0.0001). At 5 and 10 years from diagnosis, the probability of MACE-free survival was 89.39% and 68.77% respectively in the anti-MPO ANCA group, and 93.39% and 83.36% in the anti-PR3 ANCA group (p=0.0001) (figure 1).
The incidence rate of MI was 6.16 per 1000 patient-years in the anti-MPO ANCA group, compared to 4.09 per 1000 patient-years in the anti-PR3 ANCA group. The mean time to MI occurrence was 2.21 (SD: 1.81) years in the anti-MPO ANCA group, while it was 4.24 (SD: 6.11) years in the anti-PR3 ANCA group (p=0.0001). At 5 and 10 years from diagnosis, the incidence of MI was 4% in the anti-MPO ANCA group, compared to 2% and 3%, respectively, in the anti-PR3 ANCA group (p=0.31).
The incidence rate of stroke was 6.13 per 1000 patient-years in the anti-MPO ANCA group, compared to 2.72 per 1000 patient-years in the anti-PR3 ANCA group. The mean time to stroke occurrence was 4.39 (SD: 2.99) years in the anti-MPO ANCA group, while it was 7.69 (SD: 7.42) years in the anti-PR3 ANCA group (p=0.0009). At 5 and 10 years from diagnosis, the incidence of stroke was 2% and 3%, respectively, in the anti-MPO ANCA group, and 1% and 2% in the anti-PR3 ANCA group (p=0.18).
The Cox regression model found an association between the presence of anti-MPO ANCA and the risk of MACE (HR: 1.77; 95% CI: 1.13-2.8; p=0.0134). A similar trend was observed for the risk of stroke (HR: 3.05; 95% CI: 0.88-10.6; p=0.0795). There was no association found between the presence of anti-MPO ANCA and the risk of MI.
Conclusion: Patients with anti-MPO ANCA appear to be at higher risk of MACE.
To cite this abstract in AMA style:
Idoate J, Mourguet M, David R, Faguer S, Huart A, Chauveau D, Villeneuve T, Prevot G, Guilleminault L, Mouchon E, Balardy L, Sailler L, De Almeida Chavez S, Alric L, Michaud M, Lairez O, Pugnet G. Impact of ANCA Specificity on Risk of Major Adverse Cardiovascular Events in ANCA-associated Vasculitis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/impact-of-anca-specificity-on-risk-of-major-adverse-cardiovascular-events-in-anca-associated-vasculitis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-anca-specificity-on-risk-of-major-adverse-cardiovascular-events-in-anca-associated-vasculitis/