Session Information
Date: Sunday, November 5, 2017
Title: Education Poster
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Although much emphasis is focused on lung ultrasonography(US) within the critical care field, there is a growing interest in the use of lung US and its role in diagnosis and monitoring of Interstitial Lung Disease(ILD). A large burden of ILD is attributed to connective tissue disorders(CTD) and often presents symptomatically after irreversible fibrosis has ensued. With increasing use of point-of-care musculoskeletal US among rheumatologists, translation of this expertise towards lung US places the rheumatologist in a unique position to screen for asymptomatic lung involvement among patients with CTD. Despite recent evidence of the feasibility and utility of using lung US in screening of patients with CTD-ILD, the field is relatively immature and standardized training curriculum for the rheumatology community is lacking. The aim of this study is to determine the effectiveness of a formalized lung US training course for Rheumatology fellows and attending physicians in incorporating and improving skills and attitudes in lung US.
Methods: Four rheumatology fellows and four board-certified rheumatologists were enrolled in a 4-hour training session including didactics, live models and simulation experience. Pre-course, post-course and 6-month follow-up surveys evaluated participant perceptions towards previous US experience, training, clinical utility and attitudes toward dedicated lung US. Written exams (21 multiple-choice questions) were completed before, after training, and at 6 months to evaluate basic knowledge in ultrasound physiology, lung US anatomy, artifact and pathology recognition. In addition, a 30-point practical exam using live models and simulation, evaluated competency in machine setup, anatomical, artifact and pathology recognition
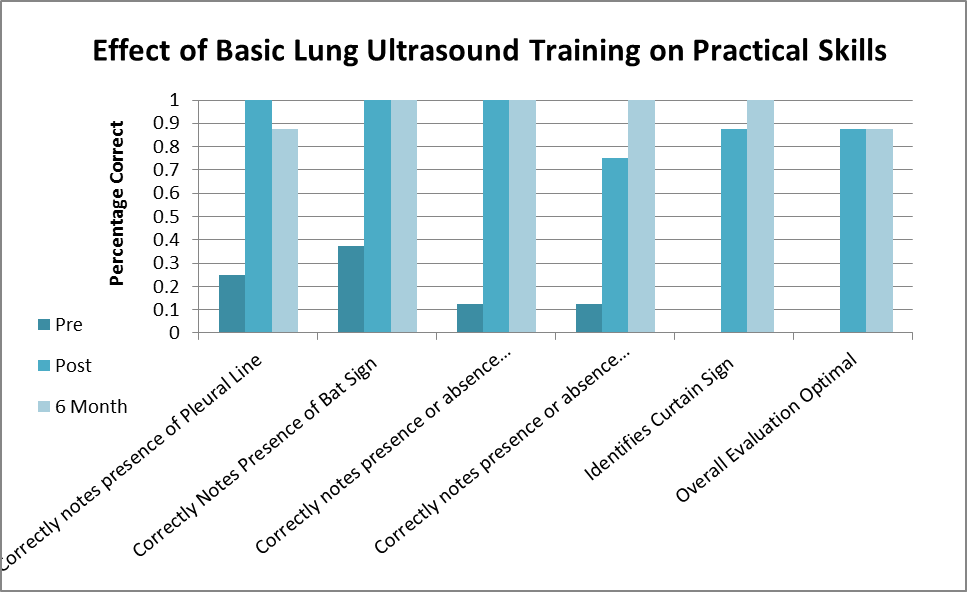
Results: The results of this study show overall improvement in written test scores ( 43% v 66% p<0.001) Considerable improvement was also noted in overall practical skill score following training course. ( 16.8% v. 93.4% p<0.001). Sub category improvements were seen in ultrasound setup and anatomical landmark identification (18.8% v 94.4% p<0.001 ) identification of pulmonary artifact (15.6% v 91% p<0.001) and pulmonary pathology identification (29% v. 91% p<0.001). 6 month retention rate was excellent for: Written Scores ( 92.3%) , Practical Skills (93%) , Setup/Landmark Identification (88%) Artifact Identification (100%).
Conclusion: Dedicated lung ultrasonography training can be integrated into a rheumatology fellowship program for potential screening of CTD-ILD.
To cite this abstract in AMA style:
Gasho C, Torralba K, Chooljian D, Wang CB, Dinh V. Impact of a Lung Ultrasound Course for Rheumatology Specialist (IMPACT-2) [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/impact-of-a-lung-ultrasound-course-for-rheumatology-specialist-impact-2/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-a-lung-ultrasound-course-for-rheumatology-specialist-impact-2/