Session Information
Date: Monday, November 18, 2024
Title: RA – Treatment Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with RA are at increased risk of serious infection, but less is known about common, non-serious infections. Our prospective study aimed to assess associations between medications for RA and the risk of common infections.
Methods: We remotely recruited adults with RA with current DMARD use July 2022-July 2023 who were patients in the Excellence Network in RheumatoloGY (ENRGY), a national community rheumatology practice-based research network (PBRN). Participants joined the ArthritisPower Registry (now PatientSpot) using a smartphone or computer and completed a baseline and up to 6 monthly follow-up surveys, reporting medications, patient-reported outcomes, flares, and infections in the preceding 30 days. Using data from consecutive monthly surveys and excluding those with ongoing infection at the prior survey, associations between medication use at the prior survey and infection at the subsequent survey were evaluated using logistic regression with generalized estimating equations to account for multiple observations per participant, adjusting for confounders. Patients receiving a csDMARD without a concomitant biologic/JAKi were divided into biologic/JAKi naïve (no prior use) vs. experienced given differences in observed infection risk.
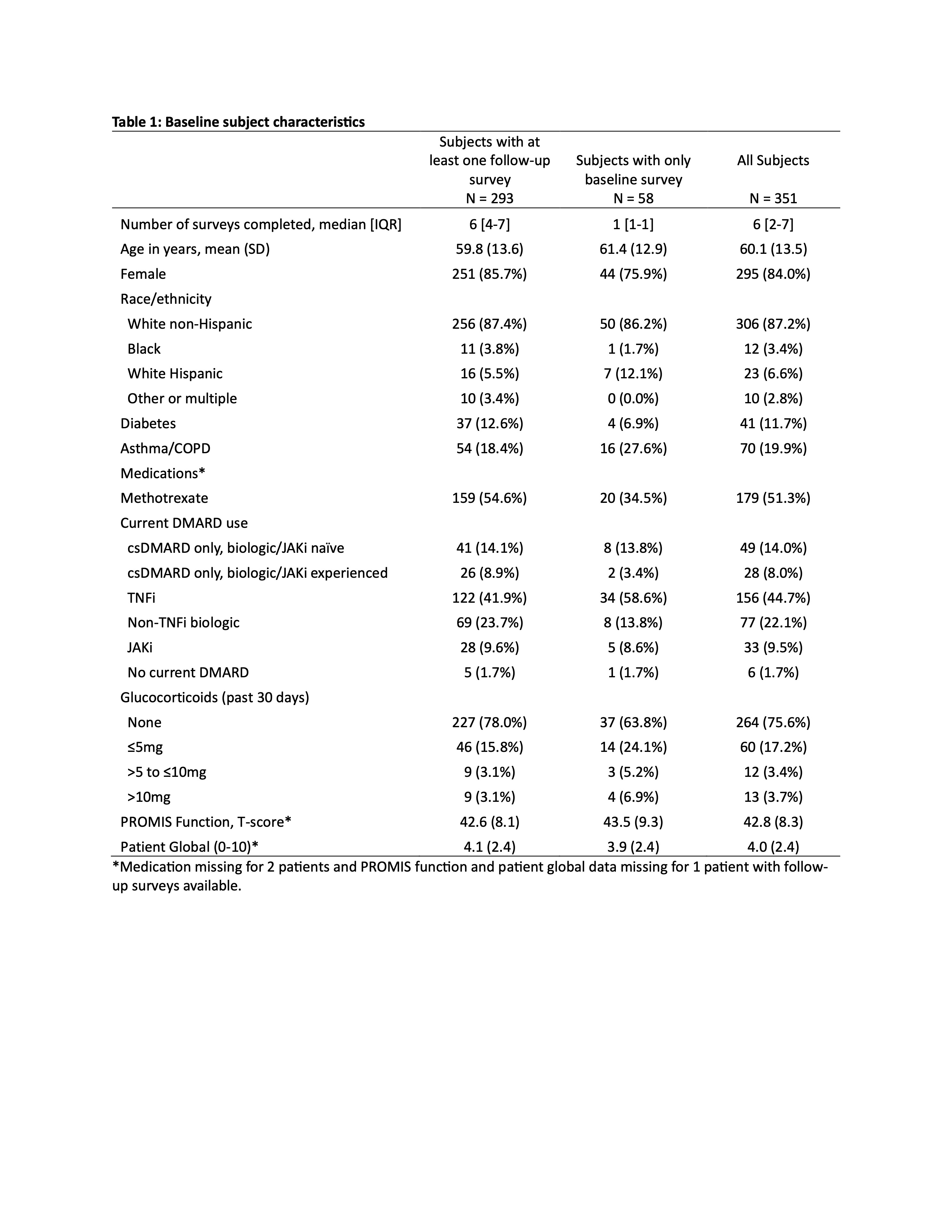
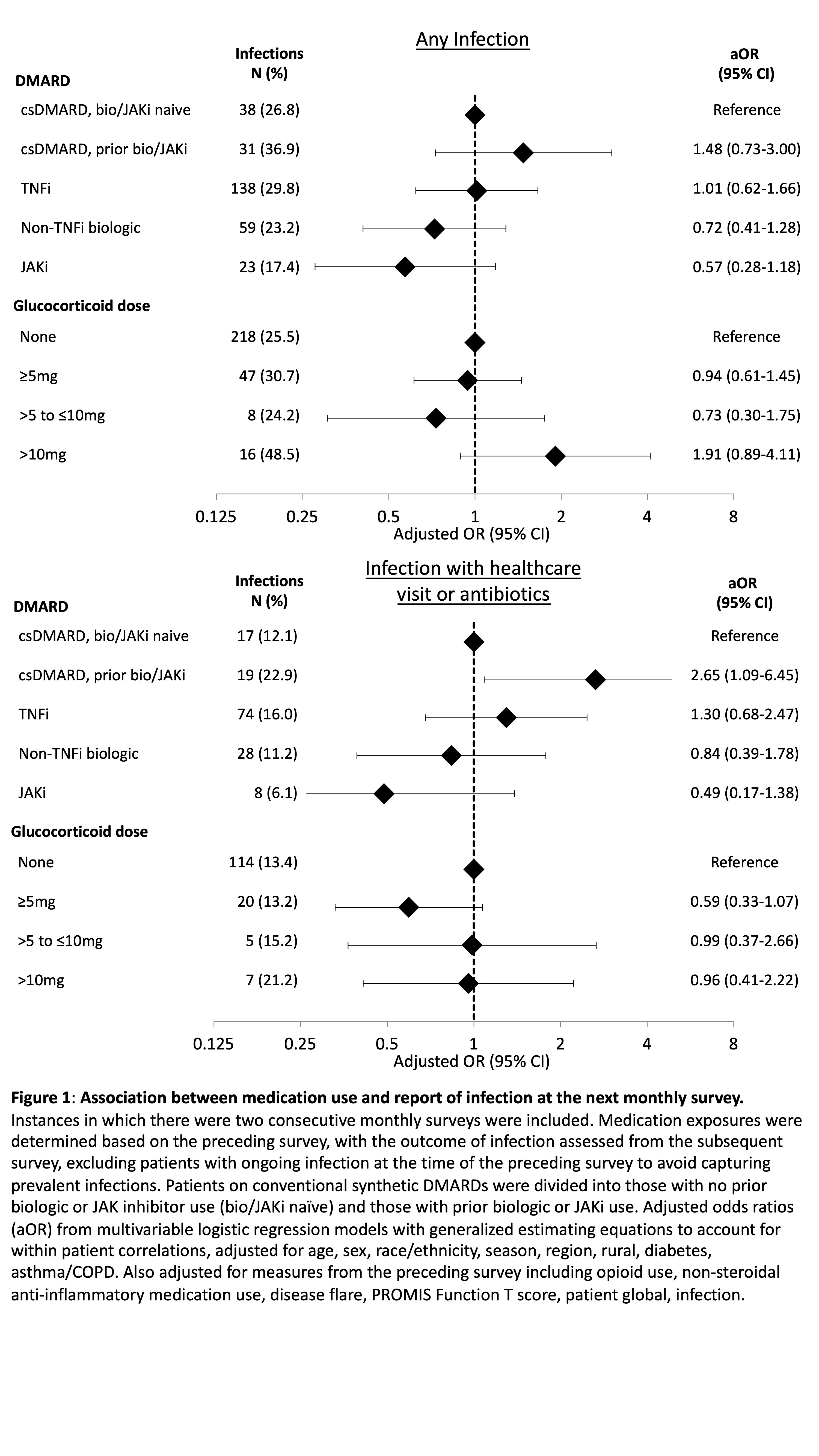
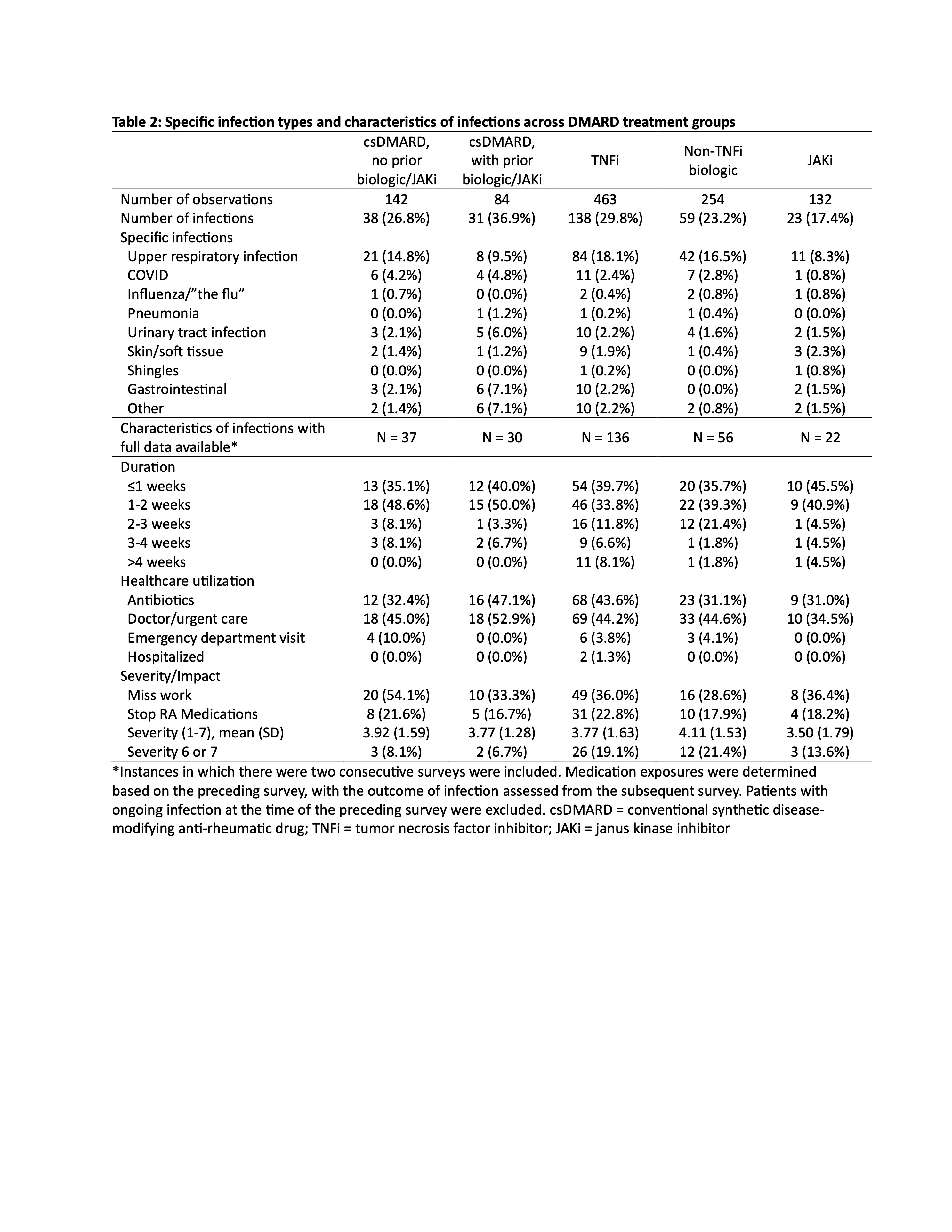
Results: We recruited 351 patients with RA (98% confirmed by EHR diagnosis), with 293 completing ≥1 follow-up survey (Table 1). Mean age was 60; 84% were female, 87% non-Hispanic White (Table 1). At baseline, 78% were receiving a biologic or JAKi, most commonly a TNF inhibitor, and 22% were on csDMARDs alone (83% methotrexate). Glucocorticoids were used by 24%, with most (71%) on ≤5mg/day. After excluding 84 infections due to report of ongoing infection the previous month, we identified 439 infections (28% of monthly observations, 3.3 infections/patient-year). Associations between medication use and infection were assessed among 1075 qualifying observations with 289 (27%) total infections and 146 (14%) infections with healthcare encounter or antibiotic use. Compared to those receiving csDMARDs who were biologic/JAKi naïve, current biologic or JAKi use was not associated with either infection outcome; rates of both outcomes were highest among biologic/JAKi experienced patients currently on csDMARDs alone (Figure 1). Infections were more common in those using glucocorticoids ≥10mg/day, but associations were not significant in adjusted models. Winter season, rural residence, lower PROMIS Function, and previous infection were associated with increased risk for one or both infection outcomes (not shown). Characteristics of infections including severity and healthcare utilization were similar across treatment groups (Table 2).
Conclusion: Infections are common in patients with RA. We did not find an increase in the risk for infections in patients receiving biologics, JAKi, or low-dose glucocorticoids, and our results suggest that exposures and comorbidities may have a stronger effect than these therapies on the risk of non-serious infections. Studies are needed to determine whether interrupting medications in patients with infection improves or worsens RA-related and infectious outcomes.
To cite this abstract in AMA style:
George M, Gavigan K, Venkatachalam S, Curtis D, Stradford L, Nowell W, Xie F, Baker J, Curtis J. Immunosuppressive Medications and Common Infections in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/immunosuppressive-medications-and-common-infections-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/immunosuppressive-medications-and-common-infections-in-patients-with-rheumatoid-arthritis/