Session Information
Date: Monday, November 14, 2022
Title: T Cell Biology and Targets in Autoimmune and Inflammatory Disease Poster
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with immune-mediated rheumatic diseases (IMRDs) are commonly treated with immunosuppressors and prone to infections. Recently introduced mRNA SARS-CoV-2 vaccines have demonstrated extraordinary efficacy across all ages. Immunosuppressed patients were excluded from phase III trials with SARS-CoV-2 mRNA vaccines. We aim to fully characterise B-cell and T-cell immune responses elicited by mRNA SARS-CoV-2 vaccines in patients with rheumatic diseases under immunotherapies, and to identify which drugs reduce vaccine’s immunogenicity.
Methods: Humoral, CD4 and CD8 immune responses were investigated in 100 naïve patients with SARS-CoV-2 with selected rheumatic diseases under immunosuppression after a two-dose regimen of SARS-CoV-2 mRNA vaccine. Responses were compared with age, gender and disease-matched patients with IMRD not receiving immunosuppressors and with healthy controls.
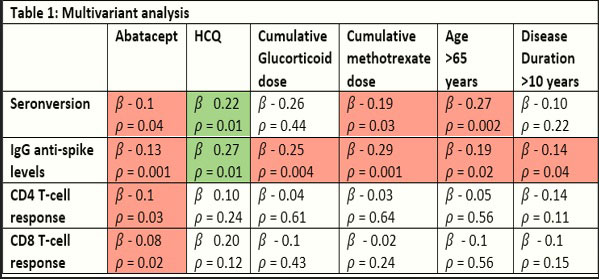
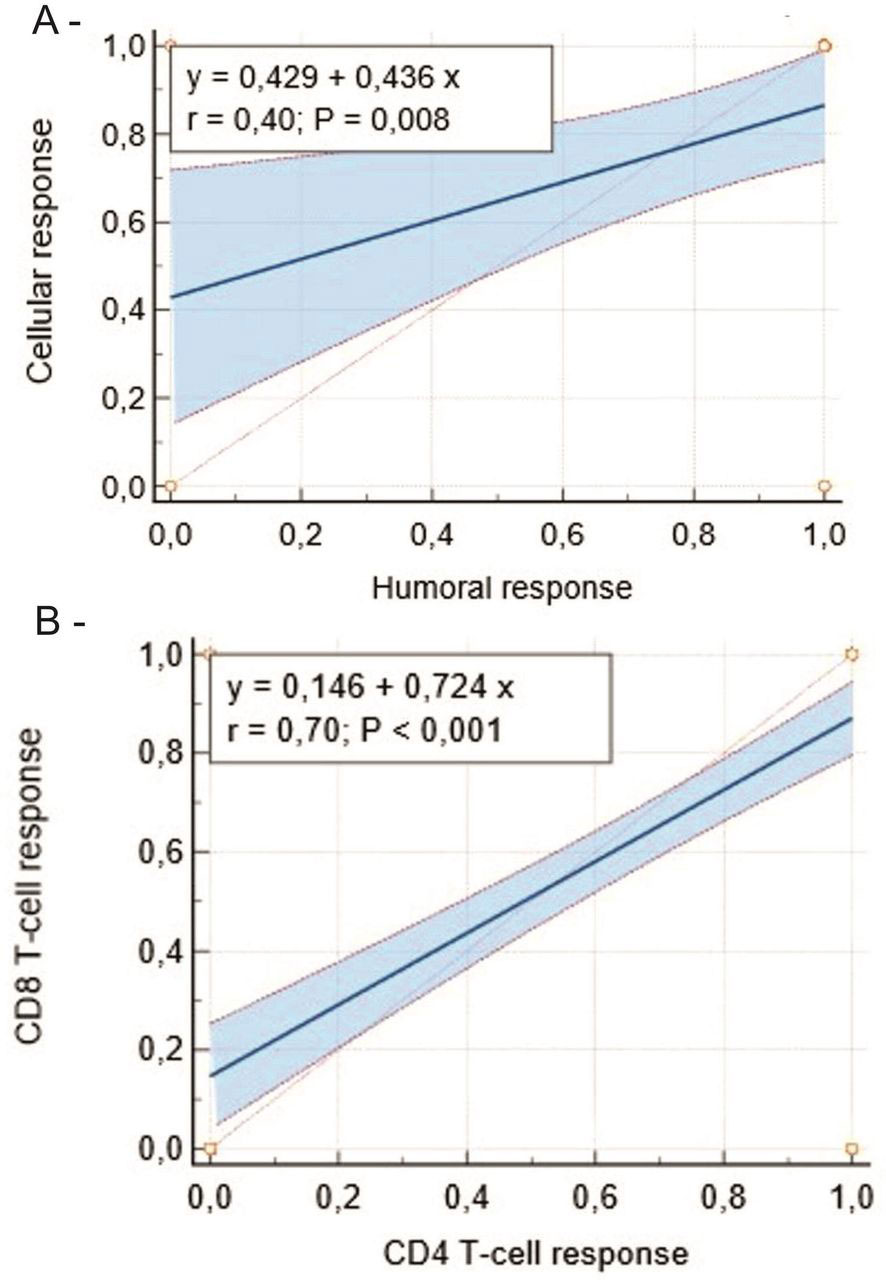
Results: Patients with IMRD showed decreased seroconversion rates (80% vs 100%, p=0.03) and cellular immune responses (75% vs 100%, p=0.02). Patients on methotrexate achieved seroconversion in 62% of cases and cellular responses in 80% of cases. Abatacept decreased humoral and cellular responses. Rituximab (31% responders) and belimumab (50% responders) showed impaired humoral responses, but cellular responses were often preserved. Antibody titres were reduced with mycophenolate and azathioprine but preserved with leflunomide and anticytokines.
Conclusion: Patients with IMRD exhibit impaired SARS-CoV-2 vaccine immunogenicity, variably reduced with immunosuppressors. Among commonly used therapies, abatacept and B-cell depleting therapies show deleterious effects, while anticytokines preserved immunogenicity. The effects of cumulative methotrexate and glucocorticoid doses on immunogenicity should be considered. Humoral and cellular responses are weakly correlated, but CD4 and CD8 tightly correlate. Seroconversion alone might not reflect the vaccine’s immunogenicity.
To cite this abstract in AMA style:
Sieiro Santos C, Calleja Antolín S, Moriano Morales C, Álvarez Castro C, Díez Álvarez E, Ruiz de Morales J. Immune Responses to mRNA Vaccines Against SARS-CoV-2 in Patients with Immune-mediated Inflammatory Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/immune-responses-to-mrna-vaccines-against-sars-cov-2-in-patients-with-immune-mediated-inflammatory-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/immune-responses-to-mrna-vaccines-against-sars-cov-2-in-patients-with-immune-mediated-inflammatory-rheumatic-diseases/