Session Information
Date: Saturday, November 16, 2024
Title: Imaging of Rheumatic Diseases Poster I: Inflammatory Arthritis
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Spondyloarthropathies (SpAs) are a group of seronegative, inflammatory arthritides, including axial spondylarthritis (ax-SpA), axial psoriatic arthritis (ax-PsA), and inflammatory bowel disease related arthritis with axial involvement (ax-IBD). Axial involvement is a hallmark of SpAs. While MRI criteria for ax-SpA are well established, imaging characteristics for ax-PsA and ax-IBD are less defined. Our study aims to describe the prevalence of inflammatory and structural lesions in whole spine and sacroiliac joint MRI (SIJ MRI) among patients with ax-SpA, ax-PsA, and ax-IBD and to evaluate the relationship between these lesions, clinical features, and treatment strategies at Cleveland Clinic Abu Dhabi.
Methods: Retrospective analysis of patients who had a whole spine and SIJ MRI from May 2015-Dec 2023, selected from 3 populations: (1) ax-SpA, (2) ax-PsA, (3) ax-IBD. MRI spine and/or MRI SIJ changes were defined according to the Assessment of Spondylarthritis International Society (ASAS) and radiologist impression. Demographic data: age, gender, age at diagnosis, medication, and comorbidities. Descriptive statistics were utilized for analysis.
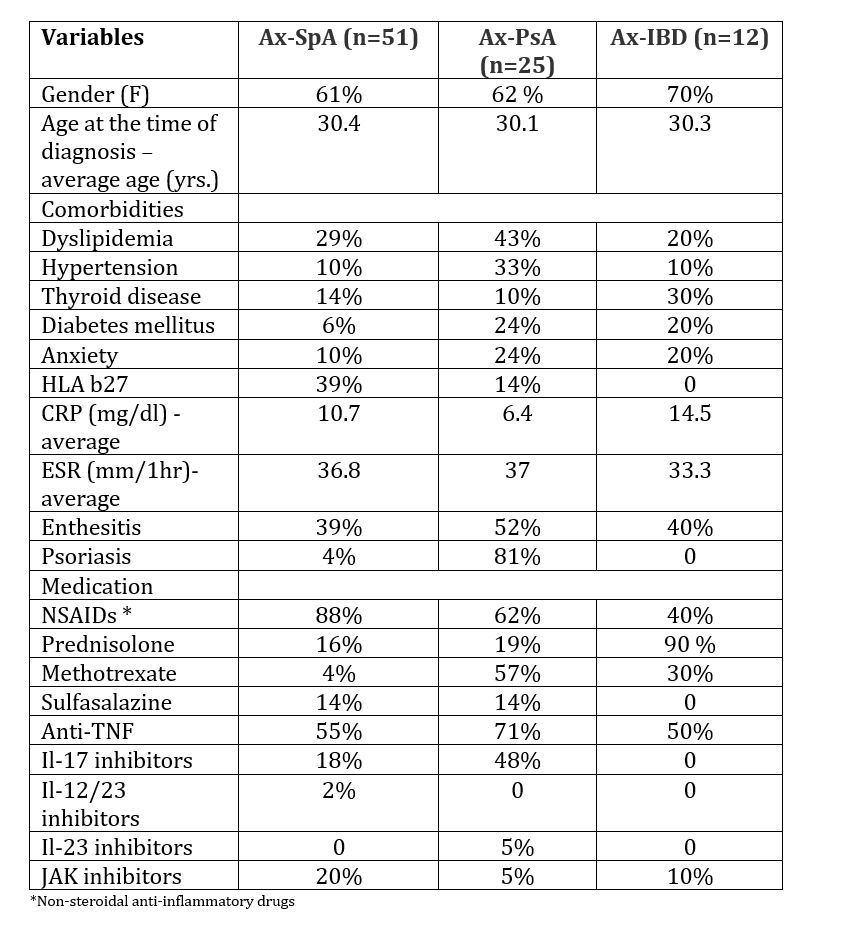
Results: 88 patients were enrolled, patients with Ax-SpA, ax-PsA, and ax-IBD (26%,62%, and 12 %, respectively, age at the time of diagnosis 30±10 (Mean±SD) years with a BMI of 28.9±5 Kg/m2. The most common comorbidities were dyslipidemia (32%), hypertension (16%), and thyroid disease (16 %). 29 % had positive HLA B27, with a mean CRP of 10±13. The most associated manifestations were enthesitis at 43 % and psoriasis at 23%. NSAIDs were used by 76% of patients, methotrexate (22%) and sulfasalazine (12%) being the most common conventional disease-modifying drugs. Among biological treatments, anti-TNF were used in 59%, Il-17 inhibitors in 23%, and JAK inhibitors in 16%. Aprelimest, Il-12/23 inhibitors, and Il-23 inhibitors each accounted for 2%, 1%, and 1%, respectively (Table 1).
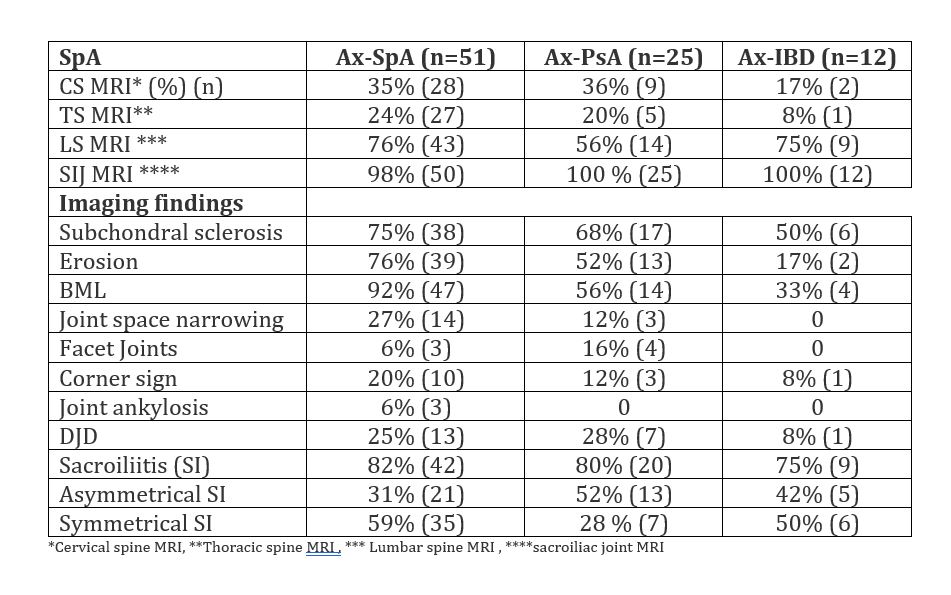
In the ax-SpA group, imaging showed that 76% had lumbar spine MRI, 35% cervical spine MRI, and 24% thoracic spine MRI, with prevalent features including bone marrow lesions (92%), erosions (76%), and subchondral sclerosis (75%). Degenerative joint disease (DJD) was less common at 25%, while sacroiliitis was positive in 82%, predominantly with symmetrical involvement (59%). In the ax-PsA group, imaging revealed lumbar spine MRI in 56%, cervical spine MRI in 36%, and thoracic spine MRI in 36%. Common findings included subchondral sclerosis (68%), bone marrow lesions (58%), and erosions (2%). Degenerative joint disease (DJD) was present in 28%. In 80% of patients, Sacroiliitis was positive, with asymmetrical involvement in the majority (52%). The ax-IBD group included 75% lumbar spine MRI, 17% cervical spine MRI, and 8% thoracic spine MRI, revealing features such as subchondral sclerosis (50%), bone marrow lesions (33%), and erosions (17%). Degenerative joint disease (DJD) was present in 8%. Sacroiliitis was positive in 75% and predominantly showed symmetrical involvement in 50% (Table 2).
Conclusion: Our study highlights specific MRI involvement patterns in SpA patients that help distinguish between subtypes such as ax-PsA, ax-SpA, and ax-IBD, thereby guiding tailored treatment.
To cite this abstract in AMA style:
Namas R, Almarzooqi A, Al Qassimi S, Memisoglu E. Imaging Characteristics and Demographic Variations in Patients with Axial Spondylarthritis, Axial Psoriatic Arthritis, and Inflammatory Bowel Disease-Related Arthritis with Axial Involvement: Insights from a Single Center at Cleveland Clinic Abu Dhabi [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/imaging-characteristics-and-demographic-variations-in-patients-with-axial-spondylarthritis-axial-psoriatic-arthritis-and-inflammatory-bowel-disease-related-arthritis-with-axial-involvement-insights/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/imaging-characteristics-and-demographic-variations-in-patients-with-axial-spondylarthritis-axial-psoriatic-arthritis-and-inflammatory-bowel-disease-related-arthritis-with-axial-involvement-insights/