Session Information
Session Type: ACR Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: 18F-flurodeoxyglucose (FDG) positron emission tomography (PET) is one of several imaging modalities used in the assessment of patients with large-vessel vasculitis (LVV). Conventionally PET images are obtained 1 hour after radiotracer injection; however, delayed imaging may be more sensitive to detect vascular inflammation.
The objectives of this study were to: 1) determine the impact of imaging acquisition time on interpretation of disease activity on FDG-PET in LVV and 2) assess the relationship between clinical features and image acquisition time.
Methods: An observational cohort of patients with giant cell arteritis (GCA) or Takayasu’s arteritis (TAK) was prospectively recruited. Patients fulfilled the 1990 ACR Classification Criteria for TAK or modified 1990 ACR Criteria for GCA. Following injection, whole-body FDG-PET magnetic resonance imaging (MRI) was performed at one-hour uptake time followed by FDG-PET computed tomography (CT) at two-hours uptake time. A single reader with vascular imaging expertise interpreted the PET studies for evidence of active vasculitis. Patients were categorized as 1) both time points active (dual active), 2) both time points inactive (dual inactive), 3) only the one-hour time point active (early time point active), and 4) only the two-hour time point active (delayed active). Imaging and clinical assessments were performed blinded to each other within a 24-hour period.
Agreement was assessed by percent agreement, Cohen’s kappa, and McNemar’s test. Nominal logistic regression was used to study factors associated with the PET categories, including age, BMI, gender, LVV type, clinical status (active/remission), ESR, CRP, and treatment status (yes/no). Significant variables in the univariable model were included in multivariable regression.
Results: 79 patients (GCA=44, TAK=35) contributed 168 paired one and two-hour PET studies. A total of 94 out of 168 scans (56%) were interpreted as active at the one-hour time point, and 129 scans (77%) were interpreted as active at the two-hour time point (p< 0.01). Scans were interpreted as both active in 90 cases and both inactive in 35 cases (percent overall agreement=74%, cohen’s kappa=0.45(fair agreement)). In discordant cases, delayed active only was observed in 39 cases versus early active only in 4 cases (McNemar’s p< 0.01).
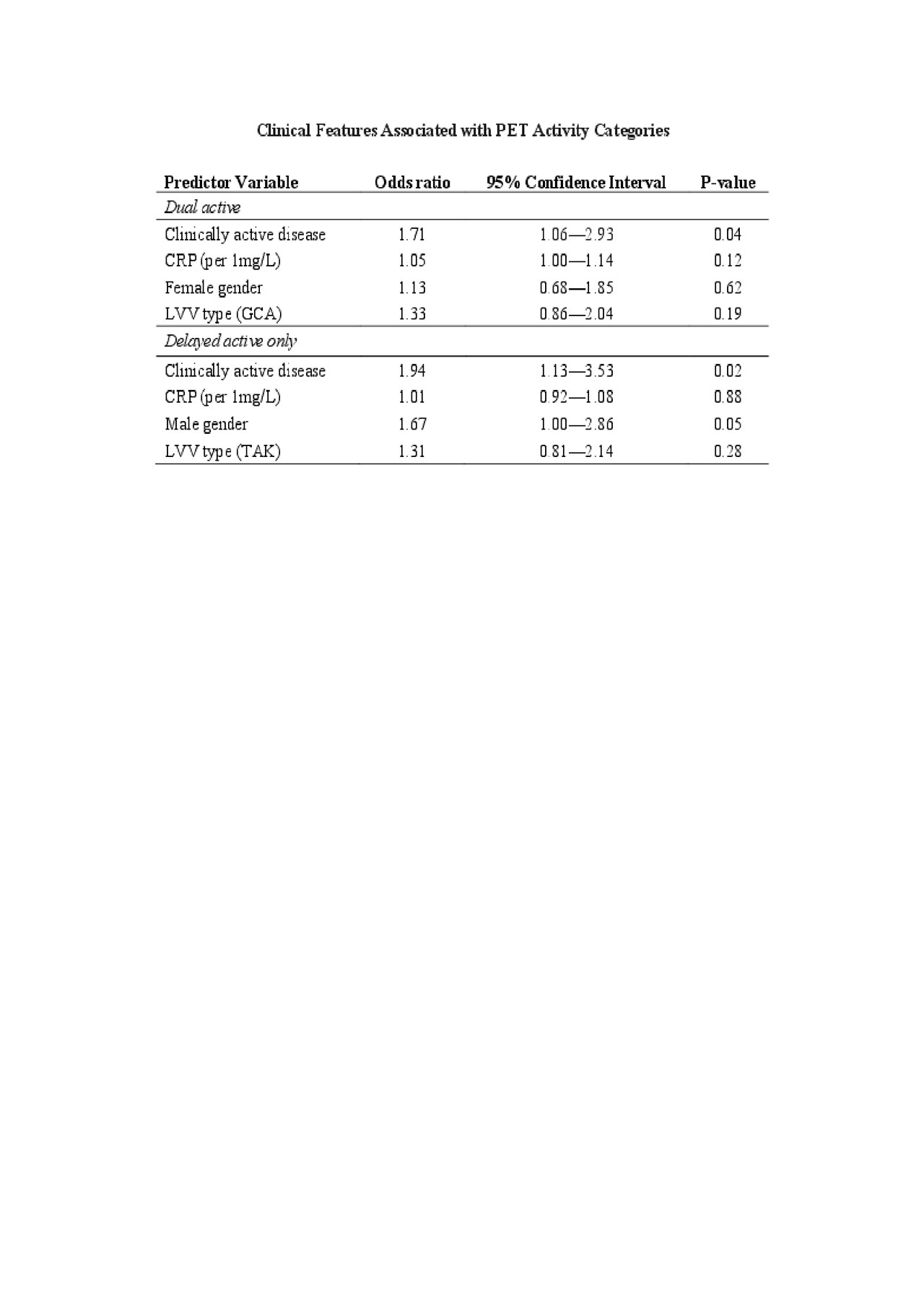
Associations between clinical variables and PET activity categories were also evaluated. Using multivariable nominal regression, clinically active disease was significantly more common in patients in the delayed active group (Odds Ratio 1.94, 95%CI 1.13 – 3.53; p=0.02) and the dual active group (Odds Ratio 1.71, 95%CI 1.06 – 2.93; p=0.04) compared to the dual inactive group as shown in Table 1.
Conclusion: Imaging protocol significantly influences interpretation of PET activity in LVV. A substantial proportion of patients with LVV had PET activity only detected by delayed imaging. These patients were significantly more likely to have concomitant clinically-determined active disease. Imaging acquisition protocols should be standardized in LVV and encourage delayed imaging.
To cite this abstract in AMA style:
Quinn K, Rosenblum J, Rimland C, Gribbons K, Ahlman M, Grayson P. Imaging Acquisition Technique Influences Interpretation of Positron Emission Tomography Vascular Activity in Large-Vessel Vasculitis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/imaging-acquisition-technique-influences-interpretation-of-positron-emission-tomography-vascular-activity-in-large-vessel-vasculitis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/imaging-acquisition-technique-influences-interpretation-of-positron-emission-tomography-vascular-activity-in-large-vessel-vasculitis/