Session Information
Date: Tuesday, October 28, 2025
Title: (1972–1989) Measures & Measurement of Healthcare Quality Poster II
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Teratogenic medications are commonly prescribed to women of reproductive age who have rheumatic conditions. Counseling on teratogenicity and contraception is critical to reducing patients’ risk of miscarriage and fetal congenital anomalies. This study assessed the frequency of rheumatologist-documented teratogenic risk counseling, gynecology referrals, and contraceptive methods among women of reproductive age on teratogenic DMARDs in an academic rheumatology clinic. Findings informed the development of a Best Practice Advisory (BPA) in the electronic medical record (EMR) with the goal of improving family planning counseling and documentation.
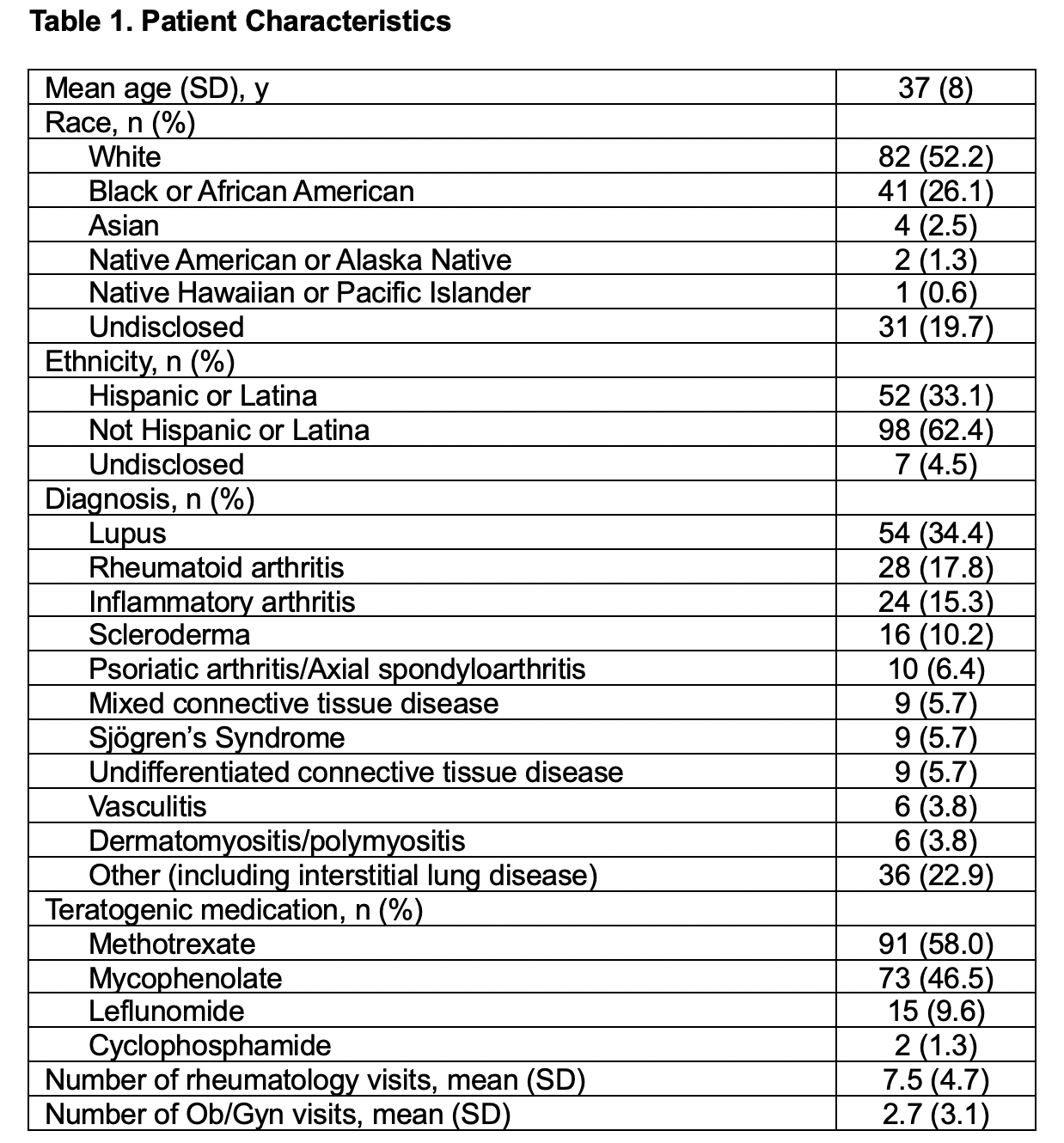
Methods: Medical records were reviewed for women aged 18–49 who attended at least one rheumatology clinic visit and were prescribed a teratogenic DMARD (methotrexate, mycophenolate, leflunomide, or cyclophosphamide). Descriptive statistics were used to analyze documentation dated between April 1, 2022, and July 31, 2024, including demographic data, clinical notes, referrals, and medication lists.
Results: We reviewed 157 patient charts. Patients had mean age 37 years (SD 8) with lupus as the most common diagnosis (Table 1). Methotrexate was the most frequently prescribed teratogenic DMARD. Over one-quarter of patients (Nf41) were not using any contraception, though 45% (Nf71) used a highly effective method (sterilization, intra-uterine device, progestin implant) (Figure 1). Documentation of teratogenic risk or contraceptive counseling in rheumatology notes was found in 34% (Nf54) and 33% (Nf52) of charts, respectively. Contraceptive counseling by Obstetrics/Gynecology (Ob/Gyn) was documented in 41% of cases (Nf65). 18% of patients (Nf28) had been referred to Ob/Gyn within the study timeframe, of whom 64% (Nf18) attended a visit and 14% (Nf4) initiated contraception. These findings informed the development of a BPA which will notify rheumatologists of patients’ teratogenic medication use, encourage appropriate documentation of counseling, and provide a one-click Ob/Gyn referral pathway with the aim of strengthening quality of care and patient safety (Figure 2).
Conclusion: This study demonstrates substantial gaps in counseling documentation, Ob/Gyn referrals, and contraception for women with rheumatic diseases on teratogenic medications. A BPA was developed in the EMR to improve patient safety and quality of care. We plan to prospectively study the impact of this intervention.
.jpg) Figure 1. Contraception Methods Among Patients Aged 18-49 at an Academic Rheumatology Clinic.
Figure 1. Contraception Methods Among Patients Aged 18-49 at an Academic Rheumatology Clinic.
Highly effective method = sterilization (hysterectomy or tubal ligation), intra-uterine device, or progestin implant. Effective method = oral contraceptive pills, depot medroxyprogesterone acetate, transdermal patch, or vaginal ring. Less effective method = condoms. Note: some patients had multiple methods documented.
.jpg) Figure 2. EMR Best Practice Advisory for Teratogenic Medication Counseling.
Figure 2. EMR Best Practice Advisory for Teratogenic Medication Counseling.
The advisory appears when rheumatologists open an encounter for female patients aged 18-49 with a teratogenic medication on their list or when they prescribe teratogenic medications for patients in this demographic. The advisory provides a one-click order for referral to the academic center’s family planning clinic. Documentation is performed directly in the alert and can be viewed in the “Flowsheets” section of the EMR. The alert will not appear if a patient’s chart contains history of tubal ligation, hysterectomy, or other surgical sterilization. Once teratogenic medication counseling is documented, the alert will stop appearing for six months, or if the rheumatologist clicks “N/A,” the alert will no longer appear.
To cite this abstract in AMA style:
Galvao R, Saklecha A, Stevenson J, Hao R, Chock E, Danve A. Identifying Gaps in Documented Contraception Counseling and Gynecology Referrals for Women on Teratogenic DMARDs: A Foundation for EMR-Based Quality Improvement [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/identifying-gaps-in-documented-contraception-counseling-and-gynecology-referrals-for-women-on-teratogenic-dmards-a-foundation-for-emr-based-quality-improvement/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identifying-gaps-in-documented-contraception-counseling-and-gynecology-referrals-for-women-on-teratogenic-dmards-a-foundation-for-emr-based-quality-improvement/