Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Despite an increasing number of therapeutic options, less than one-third of patients with PsA achieve remission. A major cause of non-response is that PsA is studied and managed as if it were a single disease, without accounting for heterogeneity in disease presentation and prognosis. Understanding heterogeneity better can improve treatment selection, shorten exposure to suboptimal therapies, reduce potential for side effects, and improve long-term outcomes. The objective of this study was therefore to identify distinct phenotypes in PsA using the PsA Research Consortium (PARC) cohort.
Methods: Baseline disease characteristics from the multicenter PsA Research Consortium (PARC) study was used to cluster PsA patients. Variable selection was performed by clinical relevance and continuous variables were standardized. Multiple Imputation by Chained Equations (MICE) was used to impute missing values. Factor analysis of mixed data (FAMD) was applied for dimensionality and collinearity reduction, followed by hierarchical clustering on the principal components to group similar patient phenotypes. The optimal number of clusters was determined by evaluating the balance between within-cluster variance reduction and between-cluster variance reduction for each level of the hierarchical clustering tree (tree method). Kruskal-Wallis and Fisher’s exact tests were performed to examine differences in continuous and categorical variables respectively across the clusters.
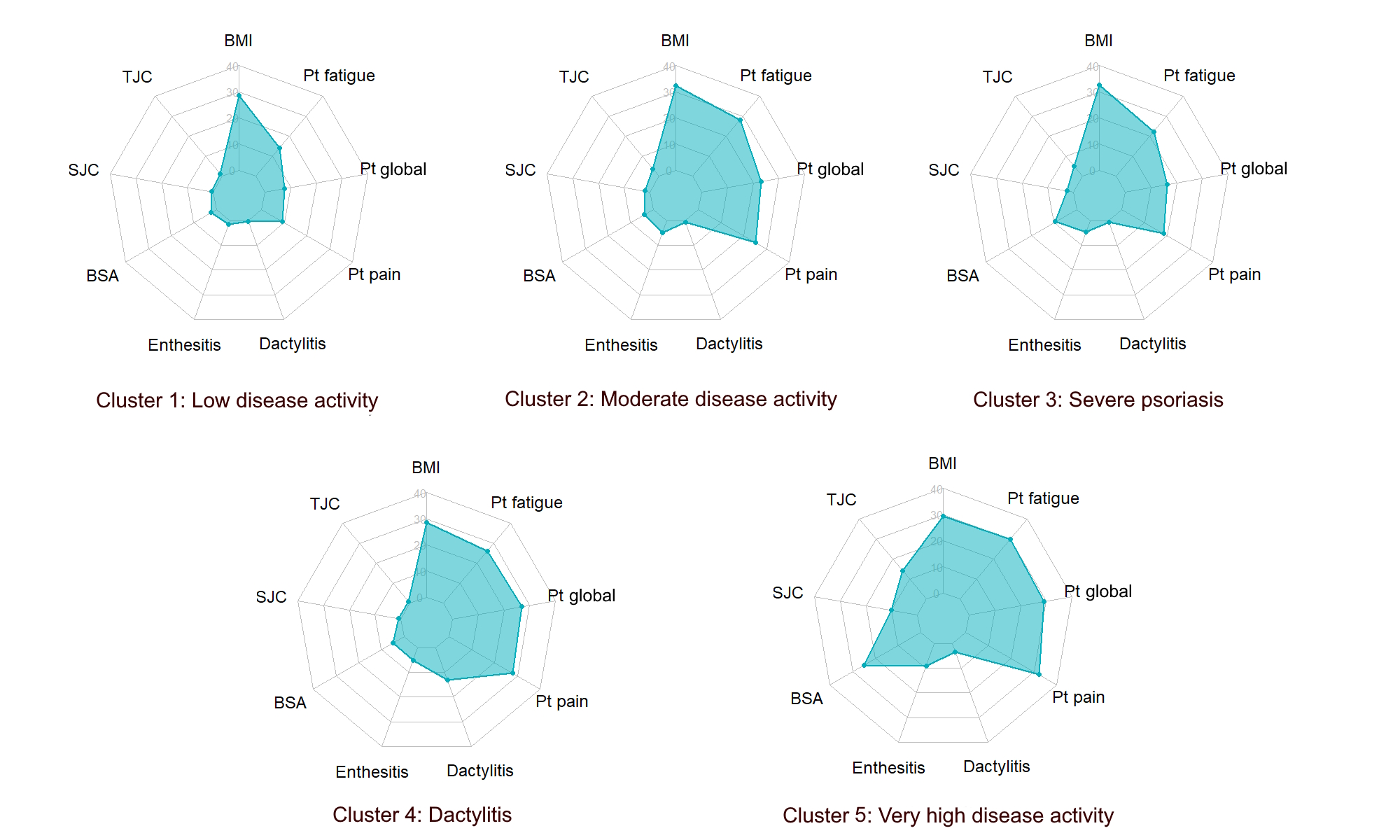
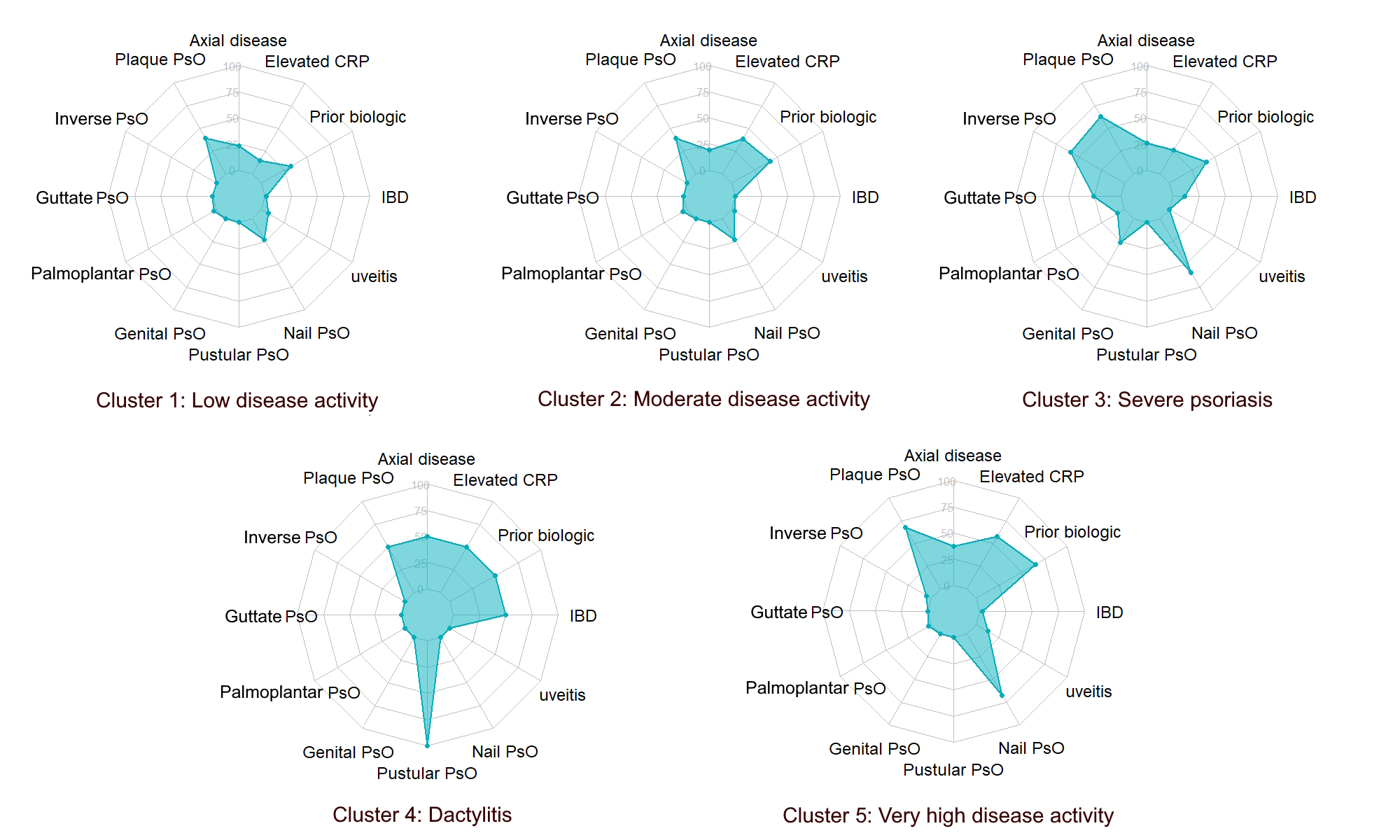
Results: In this analysis of 21 clinical variables from 529 PsA patients, five distinct phenotypic clusters were identified. The baseline characteristics of the cohort are presented in Table 1. Cluster 1 (50.09%) represented patients with low disease activity, joint counts, and PROs. Cluster 2 (36.86%) displayed moderate disease activity with higher BMI and joint counts compared to Cluster 1. Cluster 3 (5.10%) was characterized by severe psoriasis, higher guttate, palmoplantar, inverse, genital psoriasis, nail dystrophy (59.26%), and the highest mean BMI (32.44 kg/m2). Cluster 4 (0.37%) exhibited dactylitis with relatively low joint counts, but worse patient-reported outcomes (PROs). Cluster 5 (7.56%) represented very high disease activity patients with the highest joint counts, BSA, and PROs (Figures 1 & 2). The proportion of females was significantly higher in the moderate/high disease activity clusters and all patients in the dactylitis cluster were females. The very high disease activity cluster had a significantly higher proportion of non-white population (15%) compared to other clusters although overall numbers were small. The clusters were significantly different across all clustering variables except axial disease, uveitis, and palmoplantar psoriasis (p >0.05).
Conclusion: The data-driven clusters identified in this real-world study highlight the extensive heterogeneity in PsA. The variability in clinical parameters across clusters underscores the need for personalized treatment approaches in PsA, accounting for unique disease features. Future studies should focus on validating these clusters in different cohorts and exploring their application in precision medicine to transform PsA treatment paradigms.
SD, Standard Deviation; N (%), Number of patients (Percentage); BMI, body mass index; TJC, total joint count; SJC, swollen joint count; BSA, body surface area involved by psoriasis; Pt, patient; PsO, psoriasis; IBD, inflammatory bowel disease; CRP, C-reactive protein
†p-values from Kruskal-Wallis and Fisher’s exact test for continuous and categorical variables respectively
*From the BASDAI questionnaire
Missing variables: race, 47 and ethnicity, 85
Note: The variables are not standardized for better interpretability and hence on different scales plotted from 0 (lowest at the center) to maximum value for the variable (highest at the outside). Maximum value for the different variables is as follows: BMI 40, TJC 68, SJC 66, BSA 20, Enthesitis count 8 (Leeds enthesitis index + proximal plantar fascia), Dactylitis count 20, Pt pain 10, Pt global 10, and Pt fatigue 10.
Abbreviations: BMI, body mass index; TJC, total joint count; SJC, swollen joint count; BSA, body surface area involved by psoriasis; Pt, patient
Note: The variables are plotted from 0 (lowest at the center) to 100 percent (highest at the outside).
Abbreviations: PsO, psoriasis; IBD, inflammatory bowel disease; CRP, C-reactive protein
To cite this abstract in AMA style:
Karmacharya P, Byrne D, Stephens-Shields A, Crofford L, Husni M, Scher J, Craig E, Fitzsimmons R, Reddy S, Magrey M, Walsh J, Ogdie A. Identifying Distinct Phenotypes in Psoriatic Arthritis: A Study from the Psoriatic Arthritis Research Consortium (PARC) Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/identifying-distinct-phenotypes-in-psoriatic-arthritis-a-study-from-the-psoriatic-arthritis-research-consortium-parc-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identifying-distinct-phenotypes-in-psoriatic-arthritis-a-study-from-the-psoriatic-arthritis-research-consortium-parc-cohort/