Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Spinal structural damage can lead to physical dysfunction and decline of spinal mobility in patients with ankylosing spondylitis (AS). Although great progress has been made to identify potential risk factors associated with the severity of spinal structural damage, there is no definite consensus on how many factors are actually involved in its development. To yield more information, we conducted a cross-sectional study in 270 Chinese AS patients, aiming to identify potential risk factors responsible for the severity of spinal structural damage, both individually and in combination.
Methods: In total, 270 AS patients fulfilled the modified New York criteria. Computed tomography (CT) scans and lumbar/cervical X-rays were used to separately assess BASRI-SI, BASRI-hips and modified Stoke Ankylosing Spondylitis Spine Score (mSASSS), which were scored by a trained rheumatologist and a musculoskeletal radiologist where the inter-rater reliability (average kappa: 87.3%) was excellent. Spinal structural damage was appraised by mSASSS that was binarized at a cutoff of 10. Hip involvement was defined as BASRI-hips >0. Univariate and multivariate logistic regression analyses were done to identify potential risk factors for the severity of spinal structural damage, and nomogram graph was presented to facilitate clinical assessment. Statistical analyses were completed using the STATA software (v14.1) and R language (v3.5.1).
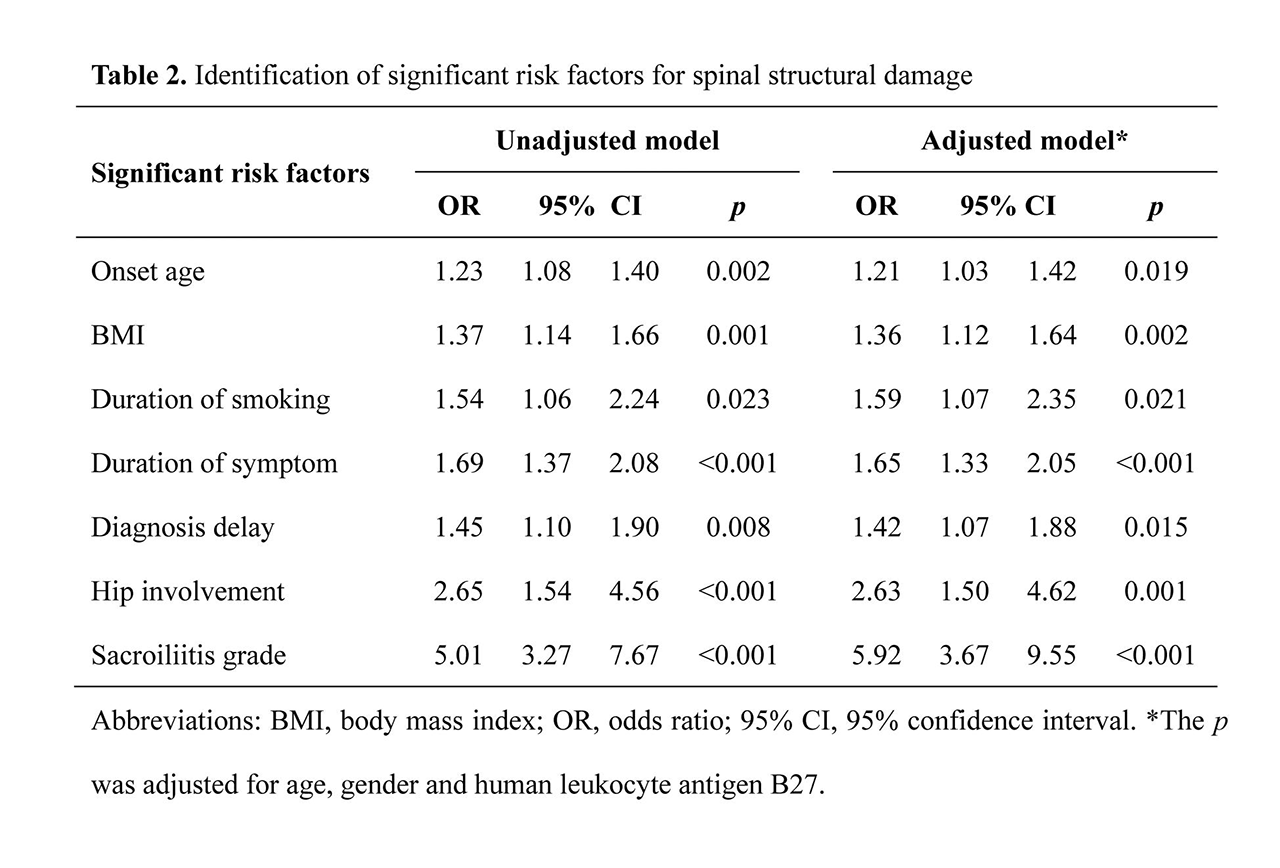
Results: 183 AS patients had mSASSS < 10 (low mSASSS), and 87 patients had mSASSS ≥10 (high mSASSS) (Table 1). Univariate analysis revealed that AS onset age, body mass index (BMI), duration of smoking, duration of symptoms, diagnosis delay, hip involvement and sacroiliitis grade were significantly associated with the risk of having high mSASSS, and all remained significant after adjusting for age, gender and HLA-B27 (all p< 0.05) (Table 2). In further analyses, hip involvement was found to be in significant interaction with BMI and duration of smoking in a graded manner. For instance, relative to patients with low BMI and negative hip involvement, those with high BMI and negative hip involvement, low BMI and positive hip involvement, and high BMI and positive hip involvement had a 1.94-, 3.29- and 5.07-fold increased risk of having high mSASSS (95% confidence interval: 0.84-4.47, 1.37-7.89, and 1.97-13.06, p=0.118, 0.008 and 0.001), respectively. To facilitate clinical assessment, a nomogram graph (Figure 1) based on 7 significant risk factors was generated with decent prediction accuracy (C-index: 0.906 and p< 0.001), and importantly besides sacroiliitis grade, onset age and BMI carried a greater weight than other risk factors.
Conclusion: We have identified seven potential risk factors responsible for the severity of spinal structural damage in Chinese AS patients. Importantly, positive hip involvement, in combination with high BMI or long duration of smoking, was associated with a remarkably increased risk of having severe structural damage in spine. Hip involvement was prevalent in our cohort and use of CT may have increased identification of hip findings compared to past studies in which X-rays were reviewed.
To cite this abstract in AMA style:
Kong W, Jefferies C, Learch T, Zhu F, Zhang N, Jin D, Zhang Y, Tao Q, Yan X, Weisman M, Ishimori M. Identification of Potential Risk Factors for Spinal Structural Damage in Chinese Patients with Ankylosing Spondylitis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/identification-of-potential-risk-factors-for-spinal-structural-damage-in-chinese-patients-with-ankylosing-spondylitis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identification-of-potential-risk-factors-for-spinal-structural-damage-in-chinese-patients-with-ankylosing-spondylitis/