Session Information
Date: Monday, November 9, 2015
Title: Spondylarthropathies and Psoriatic Arthritis - Clinical Aspects and Treatment: Clinical Aspects
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Inflammatory back pain (IBP) is regarded as an important clinical parameter of axial
spondyloarthritis (axSpA) and is often used in a
diagnostic approach. Usually symptoms of inflammatory back
pain are evaluated by a physician, however, self-evaluation of IBP
symptoms by patients might be a useful approach for self-referral of patients
and for time-saving. The aim of this study was to assess the reliability of self-evaluation
of symptoms of IBP by patients as compared to an evaluation by a physician.
Methods:
A total of 405 consecutive patients referred to a
rheumatologist because of chronic back pain starting at an age <45 years and
in whom a diagnosis of axSpA was suspected were
included in this multicentre study. A questionnaire containing 8 questions
(yes/no) relevant for IBP parameters (duration >3 months, onset prior to 45
years of age, morning stiffness of 30 minutes or longer, insidious onset of
back pain, improvement with exercise, improvement with rest, night awakening,
alternating buttock pain) were answered by the patient. The same IBP questions were then evaluated by a rheumatologist blinded for presence
or absence of other SpA-features and for the
diagnosis, and finally by a second, unblinded rheumatologist who was
responsible for the final diagnosis. The agreement among the patient and the 2 rheumatologists regarding the fulfilment of the Calin-, Berlin- and ASAS criteria were analysed.
Results:
A total of 180 patients (44.4%) were
diagnosed with definite axSpA and in 225 patients
(55.6%) SpA was excluded.
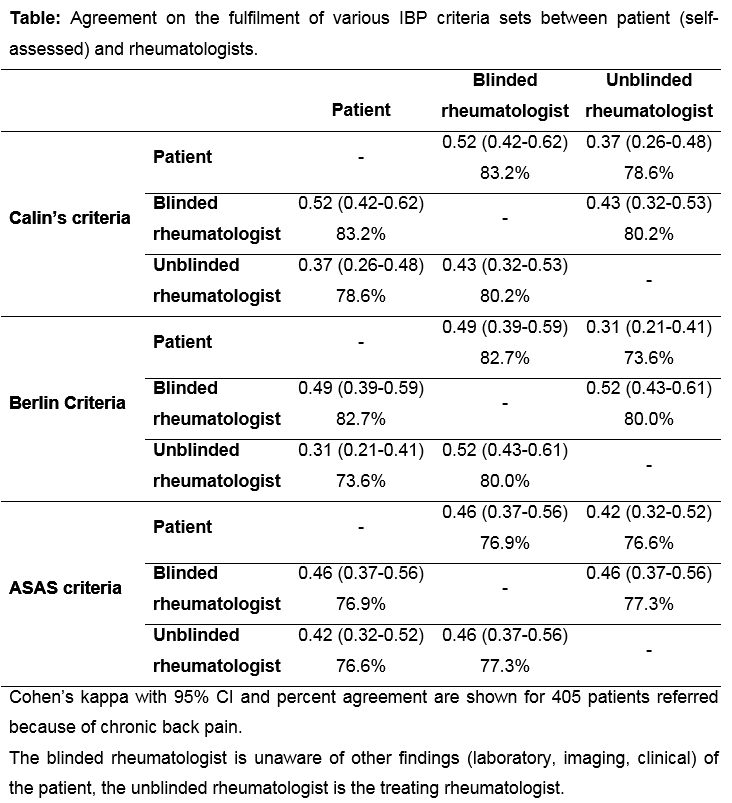
The agreement on the fulfilment of different IBP criteria sets based on
patient’s self-assessment and on the judgement of two rheumatologists (blinded
and unblinded) is presented in table. As reflected by
the kappa-values, there was a moderate agreement on the fulfilment of IBP
criteria between the patient and the blinded rheumatologist and fair to
moderate between the patient and the unblinded (diagnosing) rheumatologist. The
percentage agreement on the presence/absence of IBP was consistent and varied
between 73% and 83%. Interestingly, nearly a similar level of agreement was observed between blinded and unblinded rheumatologists.
The most consistent agreement results were obtained
for the ASAS IBP criteria. Regarding single IBP items, there was a moderate
agreement (kappa between 0.4 and 0.6) between patient’s
and rheumatologist’s judgement for the majority of items with a trend for a
better agreement between the patient and the blinded rheumatologist (as opposed
to the unblinded one).
Conclusion:
The level of agreement between
patient and rheumatologist regarding the assessment of IBP was acceptable. Patient’s self-reporting of IBP might be used in daily clinical practice.
To cite this abstract in AMA style:
Poddubnyy D, Spiller I, Sieper J, Rudwaleit M. How Reliable Is Self-Evaluation of Symptoms of Inflammatory Back Pain By Patients? [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/how-reliable-is-self-evaluation-of-symptoms-of-inflammatory-back-pain-by-patients/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/how-reliable-is-self-evaluation-of-symptoms-of-inflammatory-back-pain-by-patients/