Session Information
Date: Saturday, November 6, 2021
Title: Health Services Research Poster I: Lupus, Inflammatory Arthritis, & More (0128–0148)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic autoimmune multiorgan disease associated with significant morbidity and mortality. Although the survival rate for SLE patients has improved, hospitalization rates and healthcare utilization among SLE patients remain higher than the general population. By using a population-based cohort, we describe hospitalization rates, causes and risk factors among SLE patients compared to non-SLE patients between 2015 and 2020.
Methods: Using an established population-based research infrastructure that links the medical records of all individuals in a geographically well-defined 27-county US population, we identified SLE cases meeting the 2019 ACR/EULAR classification criteria. SLE patients who were residents in the 27-county region on January 1, 2015 were included. Patients with SLE were matched by age, sex, race/ethnicity and county of residence to non-SLE patients and were followed until 12/2020. Variables included were age, sex, race/ethnicity, number of hospitalizations, length of stay (LOS) and primary discharge diagnosis. Chi-square and Kruskal-Wallis rank sum tests were used to assess difference in characteristics between cases and controls. Hospitalization data were analyzed using person-year methods and rate ratios were obtained from Poisson models.
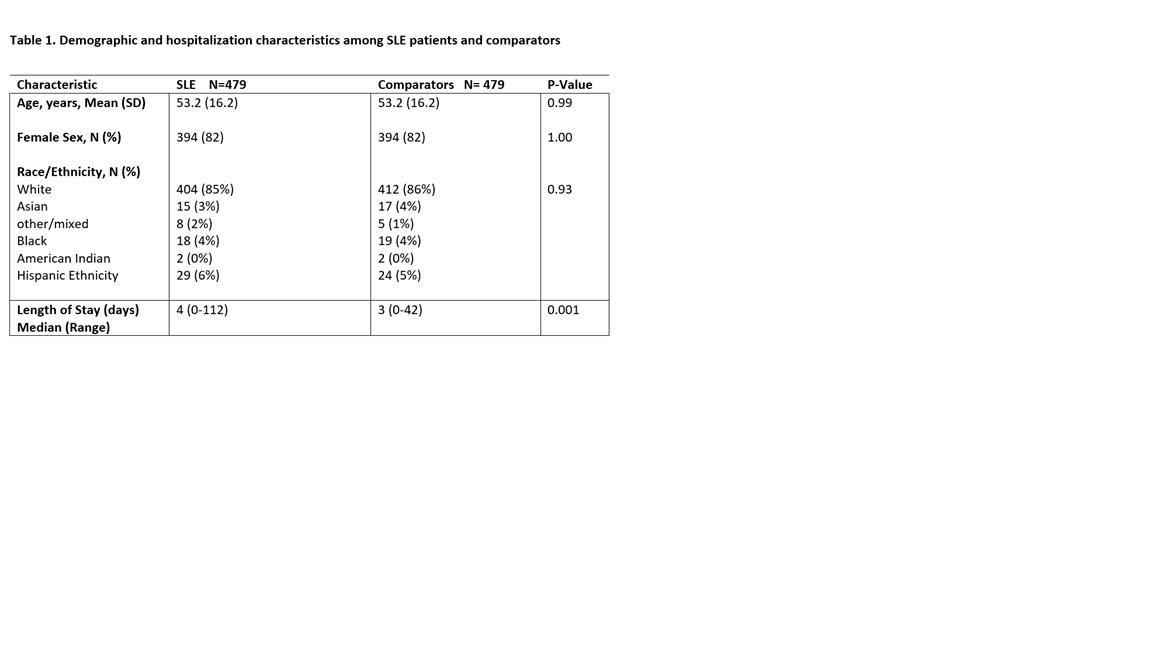
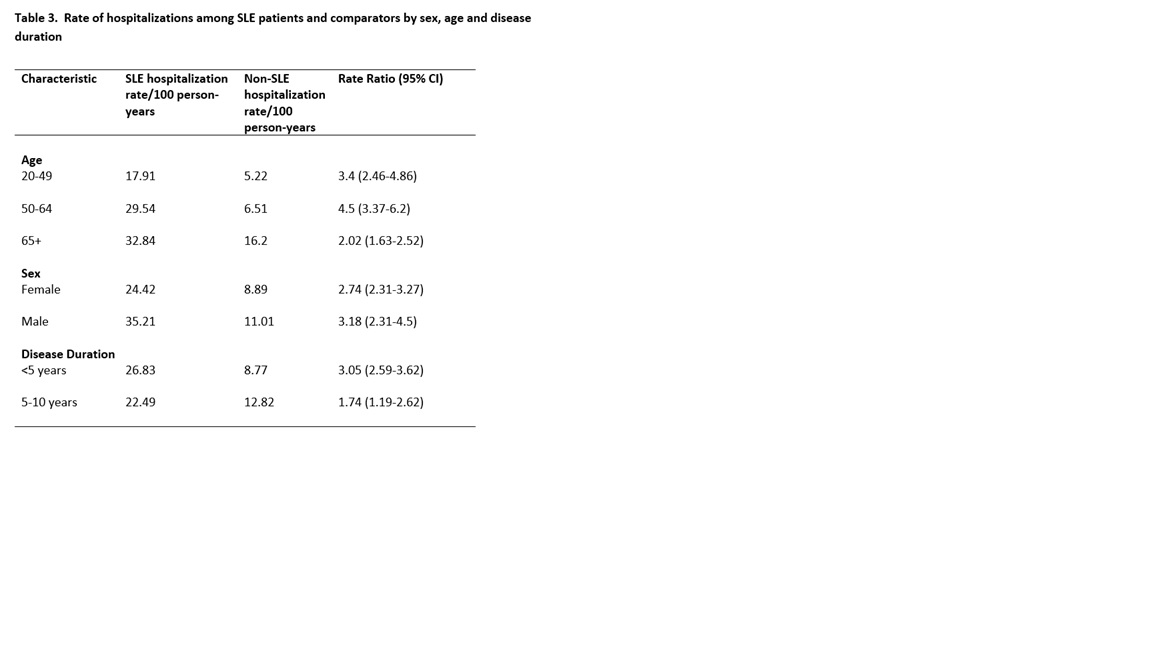
Results: We identified 479 SLE patients and 479 comparators. Mean age of SLE patients was 53.2 (SD 16.2) years, 82% were females and 85% were white (Table 1). Between 2015 and 2020, the hospitalization rate of SLE patients was 26.2/100 person-years compared to 9.3/100 person-years among comparators (rate ratio (RR) 2.83; 95% confidence interval (CI) 2.43-3.31; Table 2). LOS was higher among SLE patients (median 4 vs. 3 days; p=0.001). SLE patients were hospitalized at a significantly higher rate than subjects without SLE in 10 of 15 diagnosis categories (Table 2). The highest RR was observed for hematologic diseases (RR 11.38; 95% CI 3.24-159.95) followed by respiratory diseases (RR 4.88; 95% CI 3.00-8.75) and genitourinary diseases (RR 4.73; 95% CI 2.23-12.84). SLE hospitalization rates compared to non-SLE comparators were highest among males (RR 3.18; 95% CI 2.31-4.5), those with SLE duration < 5 years since diagnosis (RR 3.05; 95% CI 2.59-3.62) and age 50-64 years (RR 4.5; 95% CI 3.37-6.2) (Table 3).
Conclusion: SLE patients had nearly 3-fold more hospitalizations than comparators with an increased risk of hospitalization for most diagnosis categories.
To cite this abstract in AMA style:
Dabit J, Hocaoglu M, Valenzuela-Almada M, Osei-Onomah S, Vallejo-Ramos S, Giblon R, Greenlund K, Barbour K, Crowson C, Duarte-Garcia A. Hospitalization Rates Among Patients with Systemic Lupus Erythematosus: A Population Based Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/hospitalization-rates-among-patients-with-systemic-lupus-erythematosus-a-population-based-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hospitalization-rates-among-patients-with-systemic-lupus-erythematosus-a-population-based-study/