Session Information
Date: Friday, March 31, 2023
Title: Poster Breakout 6 - Systemic JIA: Genomics, Transcriptomics & Disease States
Session Type: Breakout Session
Session Time: 4:30PM-5:00PM
Background/Purpose: Over the last two decades, some children with systemic juvenile idiopathic arthritis (SJIA) have developed a severe form of interstitial lung disease (ILD) termed SJIA-associated lung disease (SJIA-LD). This has paralleled increased use of biologic agents targeting IL-1 and IL-6 to treat SJIA, leading to concern that these medications might predispose to SJIA-LD. In retrospective analyses, the majority of patients with SJIA-LD have had exposure to IL-1 and IL-6 inhibitors, but interpreting the relevance of this drug exposure history is confounded by the increasingly widespread use of these agents to treat SJIA over the same time period. Carriage of HLA DRB1*15 has been reported in previous publications as a risk factor for adverse drug reactions among patients with SJIA. We performed a retrospective chart review to evaluate these factors at our center.
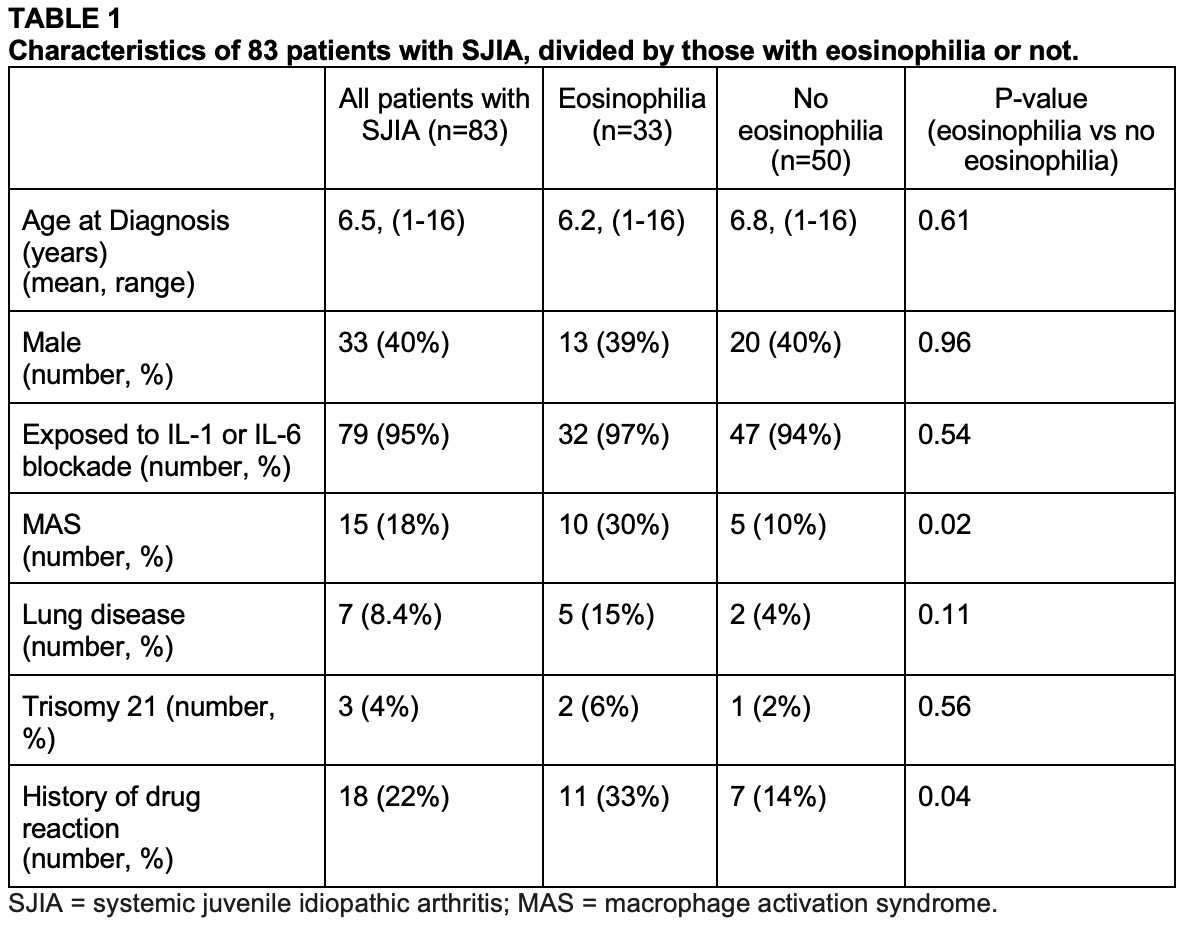
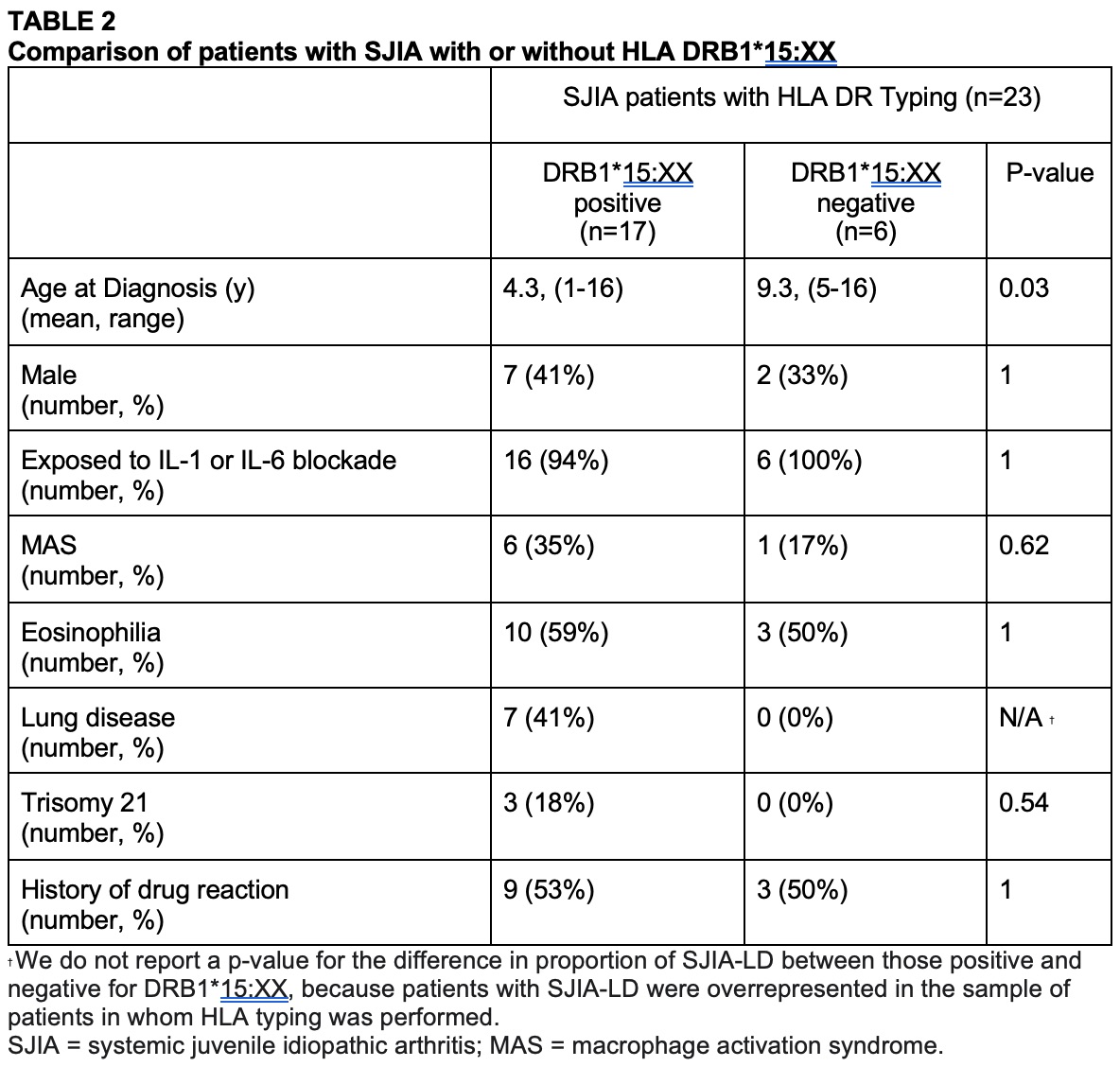
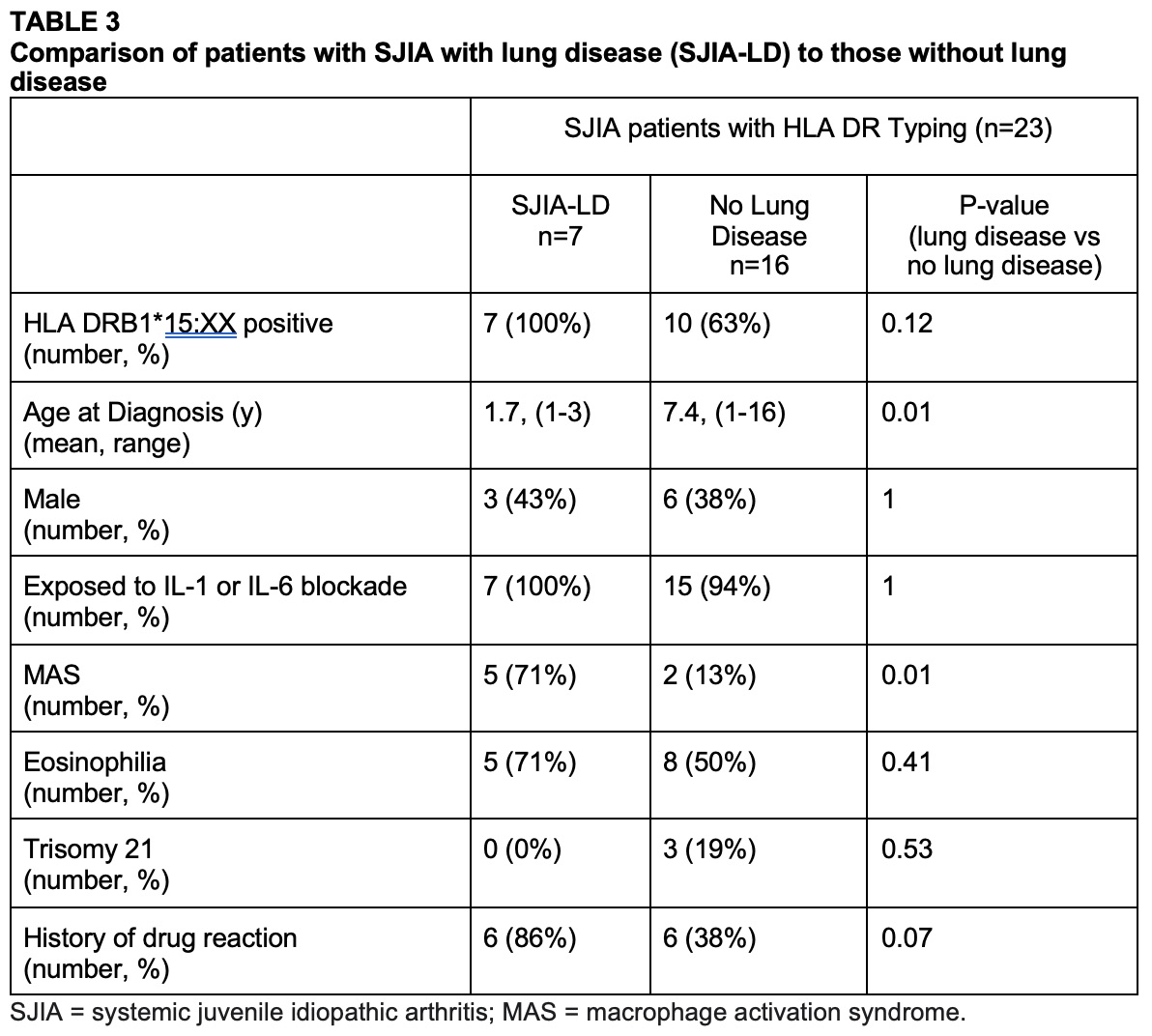
Methods: Subjects were considered for inclusion if they received a billing diagnosis code for SJIA between 1996 and 2022 (ICD-10-CM codes: M08.20, M08.2A, M08.29) before the age of 17 and had at least six months of follow-up in the University of Minnesota pediatric rheumatology clinics. Cases were then manually adjudicated to confirm the diagnosis of SJIA. 83 eligible patients were included. HLA typing wasperformed in 23 of the subjects. We compared characteristics of patients with or without eosinophilia. Among patients with HLA typing, we compared clinical characteristics of subjects with or without DRB1*15 and with or without SJIA-LD.The terminology DRB1*15:XX denotes DRB1*15:01 and DRB1*15:03. Eosinophilia was defined as an absolute eosinophil count ³700/microliter or a percent eosinophils ³10% of the white blood cell count.
Results: Exposure to IL-1 and IL-6 blockers was common, occurring in 95% of patients. Eosinophilia occurred in 40% of patients with SJIA. Eosinophilia was associated with adverse drug reactions and macrophage activation syndrome. Among the 23 patients with HLA typing, 74% carried DRB1*15, and 63% of patients without SJIA-LD carried DRB1*15. Seven subjects had SJIA-LD, all of whom carried DRB1*15 and 6 of whom had drug reactions. Patients with SJIA-LD were younger at the time of diagnosis and more likely to have had macrophage activation syndrome. There were no deaths.
Conclusion: The most striking finding in this cohort of patients with SJIA is the high rate of DRB1*15:XX carriage (74%) as compared to the general population carriage rate of 25%. Even among subjects without lung disease, the rate of DRB1*15:XX carriage was high (63%). In our cohort, all 7 patients with SJIA-LD expressed DRB1*15:XX. Eosinophilia was also common, occurring in 40% of all patients with SJIA and often prior to IL-1 or IL-6 inhibitor therapy.Eosinophilia did not differ based on the presence or absence of HLA-DRB1*15.Eosinophilia was more common among patients with severe SJIA complicated by MAS. Many patients who carried HLA-DRB1*15 did not have eosinophilia, adverse drug reactions, or lung disease despite 95% of all patients being exposed to IL-1 or IL-6 inhibitors. In our cohort, all patients with SJIA-LD expressed HLA-DRB1*15 and were also significantly younger at age of diagnosis and more likely to have had a history of MAS.
To cite this abstract in AMA style:
Lerman A, Mahmud S, Alfath Z, Langworthy B, Hobday P, Riskalla M, Binstadt B. HLA DRB1*15 and Eosinophilia Are Common Among Patients with Systemic Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/hla-drb115-and-eosinophilia-are-common-among-patients-with-systemic-juvenile-idiopathic-arthritis/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hla-drb115-and-eosinophilia-are-common-among-patients-with-systemic-juvenile-idiopathic-arthritis/