Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Hearing loss in antineutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) is one of the commonly reported manifestations of organ damage in AAV with predominantly subacute/chronic presentation. Sensorineural hearing loss has higher prevalence compared to conductive hearing loss while isolated hearing loss has been reported in 6% of AAV by Fauci et al. The present study aims to further investigate clinical characteristics and pathognomic associations of patients with sensorineural hearing loss in AAV.
Methods: This is a retrospective study design across all Mayo Clinic sites from 01/01/2020 to 08/09/2024. The study was approved by the Mayo Clinic Institutional Review Board (IRB). The patients were identified using ICD-10 diagnosis codes of ANCA associated vasculitis including granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA) or eosinophilic granulomatosis with polyangiitis (EGPA) and sensorineural hearing loss. All patients fulfilled the 2022 American College of Rheumatology (ACR)/European Alliance of Associations for Rheumatology (EULAR) classification criteria. The sample median is given for continuous variables, while categorical and ordinal variables are reported as frequency (percentage). Fisher’s exact test done for categorical variables and a Kruskal-Wallis test for continuous and ordinal variables. Statistical analyses were performed using R Statistical Software (version 4.4.1; R Foundation for Statistical Computing, Vienna, Austria).
Results: 43 unique patients were studied and demographics with clinical characteristics depicted in Table 1. GPA (76.7%) was the most common type of AAV followed by microscopic polyangiitis (MPA) (11.6%) and then eosinophilic granulomatosis with polyangiitis (EGPA) (9.3%). Patients with EGPA had a higher frequency of cochlear implants (25%) as compared to GPA (12.1%) and MPA (0%). Severe and profound hearing loss (56.1%) was the most common degree of hearing loss (Table 2). Hearing loss characteristics according to AVV demonstrated in Table 3. Patients with GPA (63.6%) had a higher percentage of severe hearing loss compared to MPA (50%) and EGPA (0%) [p=0.019]. Anti proteinase 3 antibody positive (PR3) cases had significantly more tympanometric curve type B on Audiology testing compared to myeloperoxidase (MPO) positive cases [p=0.044]. Significantly more GPA patients were treated with otic drops as compared to MPA and EGPA [p=0.046].
Conclusion: Significantly more severe sensorineural hearing loss in GPA as compared to other AAV. High rates of sensorineural loss were also noted in MPA followed by EGPA, which interestingly had a higher frequency of cochlear implants concerning for broader neurological damage. This elucidates the importance of audiology assessment in all types of AAV.
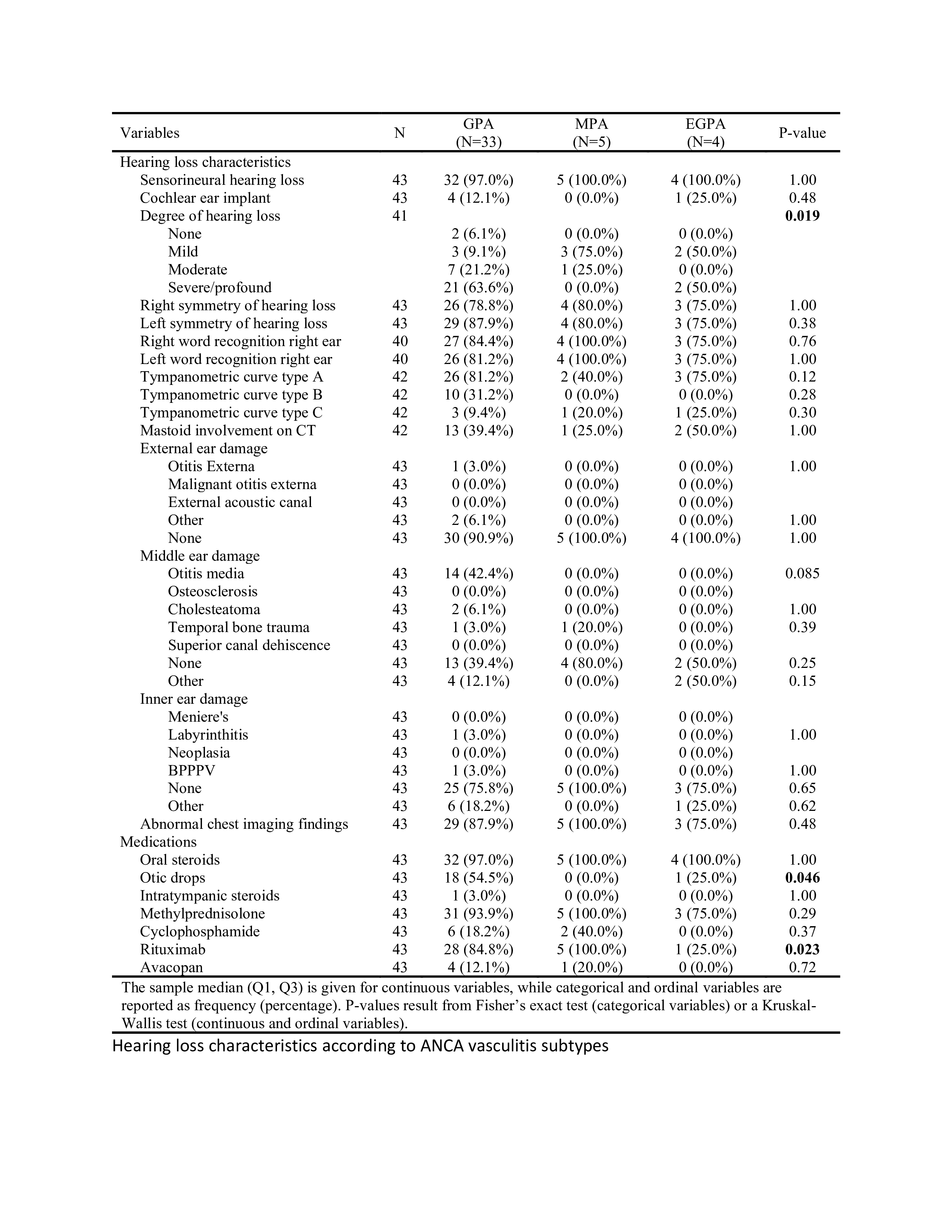 Table 1: Demographics and clinical characteristics
Table 1: Demographics and clinical characteristics
.jpg) Table 2: Hearing loss characteristics
Table 2: Hearing loss characteristics
.jpg) Table 3: Hearing loss characteristics according to ANCA vasculitis subtypes
Table 3: Hearing loss characteristics according to ANCA vasculitis subtypes
To cite this abstract in AMA style:
Mumtaz S, Fentie K, Parker J, Craver E, Majithia V, Abril A. Higher rates of severe sensorineural hearing loss in granulomatosis with polyangiitis (GPA) compared to other antineutrophil cytoplasmic antibody (ANCA) associated vasculitis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/higher-rates-of-severe-sensorineural-hearing-loss-in-granulomatosis-with-polyangiitis-gpa-compared-to-other-antineutrophil-cytoplasmic-antibody-anca-associated-vasculitis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/higher-rates-of-severe-sensorineural-hearing-loss-in-granulomatosis-with-polyangiitis-gpa-compared-to-other-antineutrophil-cytoplasmic-antibody-anca-associated-vasculitis/
