Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: To reduce the diagnostic delay in axial spondyloarthritis (axSpA), Rheumatology and Ophthalmology guidelines recommend to refer patients with acute anterior uveitis (AAU) and chronic back pain (CBP) to a rheumatologist. The impact of these recommendations in daily practice, has not yet been described. This study evaluated the prevalence of previously unrecognized axSpA in AAU patients with CBP, referred by ophthalmologists following a short instructional course to increase awareness. Secondary aims were to evaluate the timing of onset of AAU and CBP, and gender differences.
Methods: This cross sectional study included AAU patients referred with CBP (≥3 months, started < 45 years of age), from five Ophthalmology clinics. Patients with a previously diagnosed rheumatic disease, or an established other cause of AAU, were excluded. All patients underwent thorough rheumatologic evaluation, including assessment of ASAS inflammatory back pain (IBP), ASAS SpA features, laboratory examination and pelvis radiography (evaluated based on the modified New York (mNY) criteria for sacroiliitis). The primary endpoint was a clinical axSpA diagnosis (definite/possible/no axSpA), made by the rheumatologist. Patients with a definite- or possible diagnosis were classified according to the ASAS classification criteria for axSpA.
Results: Of the 101 referrals, 81 patients fulfilled the referral criteria (52% male, median age 41 years, median back pain onset 10 years before referral, Table 1). IBP was present in 53%, 56% was HLA-B27 positive, and 32% had some level of radiographic sacroiliac joint abnormalities (of whom 42% fulfilled the mNY criteria). Eventually, 23% (n=19) was clinically diagnosed with definite-axSpA (100% fulfilling the ASAS axSpA criteria; 53% radiographic) and 41% (n=33) with possible-axSpA (55% fulfilling the ASAS axSpA criteria; 6% radiographic). Importantly, of the 47 patients with recurring AAU, 87% had already had CBP during previous AAUs. Men had the same chance of fulfilling the ASAS axSpA criteria as women (57%, vs 56%), and did not differ in number of SpA features, HLA-B27, back pain duration and IBP. However, men were more likely to be clinically diagnosed with axSpA (33% versus 13% in women).
Conclusion: The referral of AAU patients with CBP resulted in 23% new axSpA diagnoses (more prevalent in men), and another 41% required follow up because of a suspicion of early axSpA. There was a substantial diagnostic delay in the majority of patients with recurring AAU, as many already had back pain during previous AAU. In AAU, screening for CBP and prompt referral has a high diagnostic yield, and should consistently be promoted among ophthalmologists and rheumatologists.
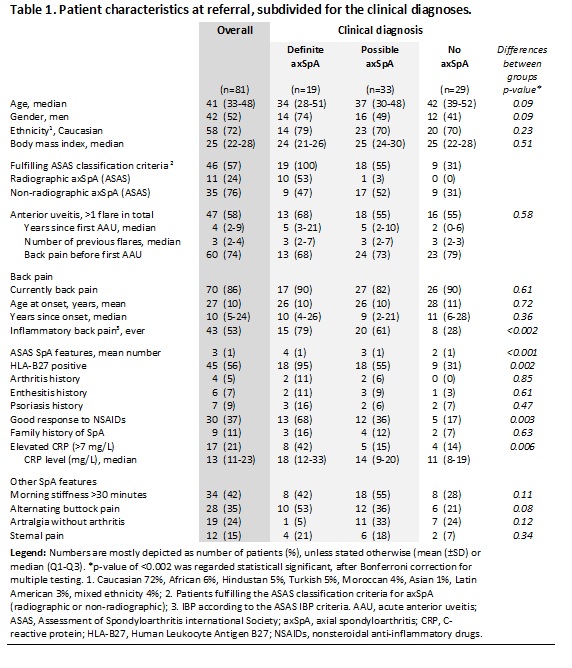 Table 1. Patient characteristics at referral, subdivided for the clinical diagnoses.
Table 1. Patient characteristics at referral, subdivided for the clinical diagnoses.
To cite this abstract in AMA style:
van Bentum R, Verbraak F, Wolf S, Boers M, Tan S, van der Horst-Bruinsma I. High Prevalence of Previously Undiagnosed Axial Spondyloarthritis in Patients Referred with Anterior Uveitis and Chronic Back Pain [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/high-prevalence-of-previously-undiagnosed-axial-spondyloarthritis-in-patients-referred-with-anterior-uveitis-and-chronic-back-pain/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-prevalence-of-previously-undiagnosed-axial-spondyloarthritis-in-patients-referred-with-anterior-uveitis-and-chronic-back-pain/
