Session Information
Date: Tuesday, November 12, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Comorbidities
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatoid arthritis (RA) are at greater risk for cardiometabolic disease and early death. It is unclear if current anti-inflammatory pharmacotherapies alone are enough to prevent RA comorbidities. In our previous work, in persons with established RA on stable medications, a high intensity interval training (HIIT) program improved both cardiorespiratory fitness and disease activity (Bartlett DB et al. Arthritis Res Ther. 2018; 20:127). To better understand the mechanisms by which exercise training improves RA inflammation and cardiometabolic risk, we evaluated relationships of HIIT-mediated changes in skeletal muscle metabolic profiles with improvements in cardiorespiratory fitness, disease activity, and systemic inflammation.
Methods: RA participants (n=11; mean age=64.0±7.5), who all satisfied 1987 ACR criteria, underwent clinical, physiologic, and biologic assessments before and after 10 weeks of supervised HIIT. Disease activity was assessed via Disease Activity Score-28 with ESR (DAS28). Cardiorespiratory fitness (relative VO2 peak, mL/kg/min) was assessed via cardiopulmonary exercise testing. Plasma concentrations of cytokines (IL-1β, IL-6, IL-8, IL-10, and TNF-α) were quantified via immunoassay. Using vastus lateralis
biopsies, skeletal muscle (m) concentrations of metabolites (organic acids, amino acids, and acylcarnitines) were quantified via targeted mass spectrometry. Percent changes for clinical and metabolic intermediate data were calculated as follows: ([post-intervention variable minus pre-intervention variable]/pre-intervention variable) × 100. Correlations were evaluated with Spearman’s rho.
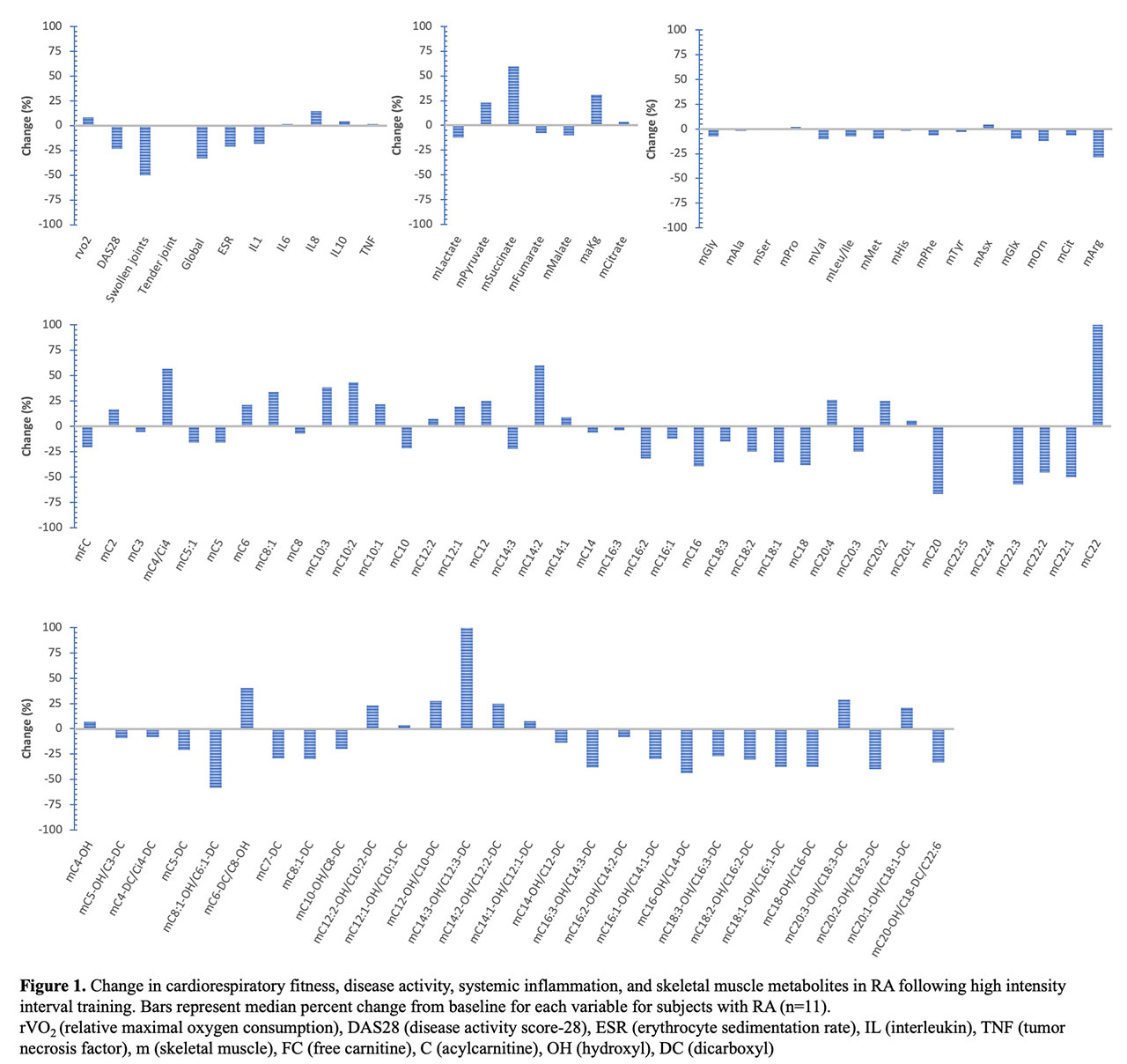
Results: In RA participants, 10 weeks of HIIT improved peak VO2 (median 8.2%) and DAS28 (median -23.8%). Changes in concentrations of plasma inflammatory cytokines and skeletal muscle organic acids, amino acids, and acylcarnitines are shown [Figure 1]. Among participants, improved peak VO2 was associated with reduced muscle concentrations of leucine/isoleucine (r=-0.65, p=0.029) and phenylalanine (r=-0.61, p=0.047). Systemic inflammation improvements were inversely related to several muscle metabolic intermediates. Improved ESR, but not DAS-28, was associated with increased muscle pyruvate (r=-0.61, p=0.046). Plasma IL-8 reductions associated with increased muscle succinate (r=-0.61, p=0.047). Plasma IL-6 reductions associated with increases in muscle citrate (r=-0.65, p=0.028) and multiple muscle acylcarnitines, including mC2 (acetylcarnitine), mC12:1, mC12, mC20:1, mC6-DC/C8-OH and mC20:1-OH/C18:1-DC (r< -0.60, p< 0.05 for all).
Conclusion: In RA, HIIT-mediated improvements in fitness and inflammation were associated with muscle metabolic changes. Cardiorespiratory fitness improvement was associated with muscle amino acid reductions. RA systemic inflammation improvements were associated with greater muscle concentrations of multiple components of oxidative metabolic machinery. Thus, RA immune and metabolic function are likely improved with exercise training through systemic enhancement of protein synthesis and fat oxidation.
To cite this abstract in AMA style:
Andonian B, Bartlett D, Muoio D, Koves T, Ilkayeva O, Hoselton A, Reaves M, Kraus W, Huffman K. High Intensity Interval Training Improves Rheumatoid Arthritis Cardiorespiratory Fitness and Systemic Inflammation in Association with Alterations in Skeletal Muscle Metabolomic Profiles [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/high-intensity-interval-training-improves-rheumatoid-arthritis-cardiorespiratory-fitness-and-systemic-inflammation-in-association-with-alterations-in-skeletal-muscle-metabolomic-profiles/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-intensity-interval-training-improves-rheumatoid-arthritis-cardiorespiratory-fitness-and-systemic-inflammation-in-association-with-alterations-in-skeletal-muscle-metabolomic-profiles/