Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus nephritis is a common feature of SLE and confers a poor prognosis. 20-50% of patients with lupus nephritis ultimately develop chronic kidney disease and renal failure in spite of efforts to induce remission of nephritis. Chronic kidney disease is epidemiologically associated with more frequent relapses and lack of remission after treatment. Both relapse and lack of remission are difficult to detect on a background of pre-existing renal disease. Proteinuria can represent residual damage. There have been intense efforts in recent years to identify urinary biomarkers, often exploiting known inflammatory features. We identified a urine biomarker that tracks proliferative aspects of lupus nephritis, HER2. This study was designed to test the sensitivity and specificity of HER2 in urine as a biomarker for active lupus nephritis.
Methods: This study design prospectively collects urine every 3 months in 100 pediatric patients with known lupus nephritis. Mean follow up at the time of writing is 3 years. Control groups include RF+ JIA, amplified pain and healthy teen females. HER2, TWEAK and VCAM are measured by ELISA. Clinical data are collected on structured CRFs at each visit. Flares of lupus nephritis are defined by SLEDAI-R (renal SLEDAI) and increased serum creatinine.
Results: Elevated urinary HER2 was observed lupus patients compared to all the control cohorts. The specificity of HER2 in lupus nephritis compared to other kidney disorders was assessed and HER2 was elevated specifically with active lupus nephritis but not vasculitis, IgA nephropathy or acute kidney injury. There was a significant association of urinary HER2 levels with SLEDAI-R by ANOVA (P< 0.0001) with a peak association with SLEDAI-R=8. When individual components of SLEDAI-R were assessed, all were associated with an increase in HER2 over non-flare patients. We validated the association of HER2 with SLEDAI-R in a cross-sectional study of adults. In the longitudinal pediatric cohort, we analyzed the subset of patients with a 1.5 fold rise in serum creatinine. HER2 was significantly elevated at the time point preceding the rise in creatinine (HER2 N-1) and at study entry (HER2 entry) for these patients (Figure 1). HER2 outperforms TWEAK and VCAM in these analyses.
Conclusion: We conclude that urinary HER2 is significantly associated with active lupus nephritis and increased levels precede flares detectable by a rise in creatinine.
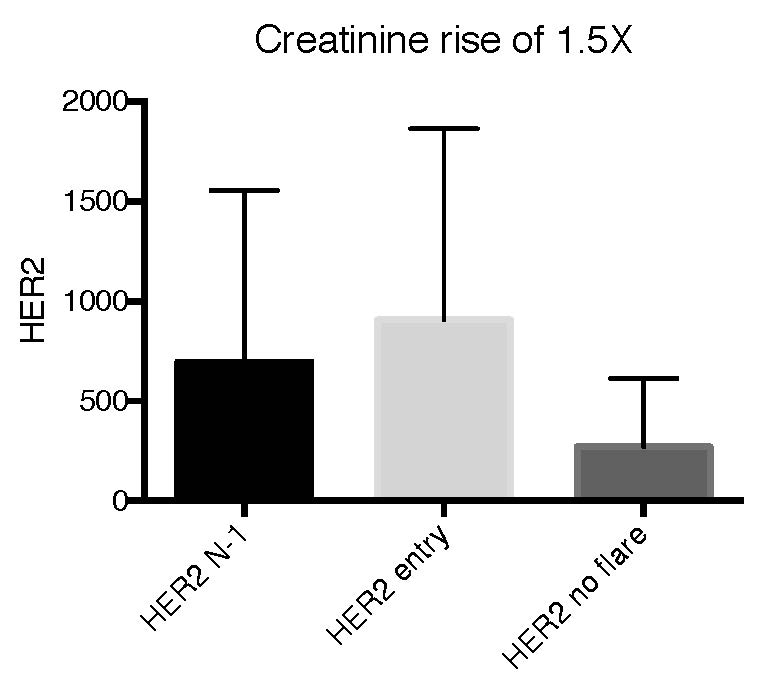
9 patients with creatinine rise of 1
To cite this abstract in AMA style:
Sullivan K, Burnham J, O'Neil K, Schanberg L, von Scheven E, Klein-Gitelman M, Costa Reis P. HER2 as a Biomarker of Proliferative Lupus Nephritis in Children [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/her2-as-a-biomarker-of-proliferative-lupus-nephritis-in-children/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/her2-as-a-biomarker-of-proliferative-lupus-nephritis-in-children/
