Session Information
Date: Sunday, October 21, 2018
Title: Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I: Comorbidities
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is associated with increased risk of coronary artery disease (CAD), but the association with heart failure (HF) is less characterized. We aimed to identify factors associated with HF risk among patients with RA.
Methods: Using the Vanderbilt University Medical Center electronic health record, we retrospectively identified 9,492 adult RA patients (median age 56 years, 76% female, 89% white) without prevalent HF at RA diagnosis. RA diagnosis was defined as ≥2 RA specific ICD-9 codes (714.0-714.2) that were ≥ 14 days apart and an anti-rheumatic medication prescription. Medication categories were: non-biologic disease modifying anti-rheumatic drug (DMARD) [azathioprine, cyclophosphamide, leflunomide, methotrexate, sulfasalazine]; anti-tumor necrosis factor (TNF) [adalimumab, certolizumab, etanercept, golimumab, infliximab]; antimalarial [chloroquine, hydroxychloroquine, quinacrine]; other biologic/small molecule DMARD [abatacept, anakinra, rituximab, tocilizumab, tofacitinib]; and systemic corticosteroid. Incident HF was defined as ≥1 ICD-9 code (428.x or 425.x) with diuretic use within 90 days. The associations between demographic, clinical factors, and medications with the risk of incident HF were quantified with multivariable-adjusted logistic regression.
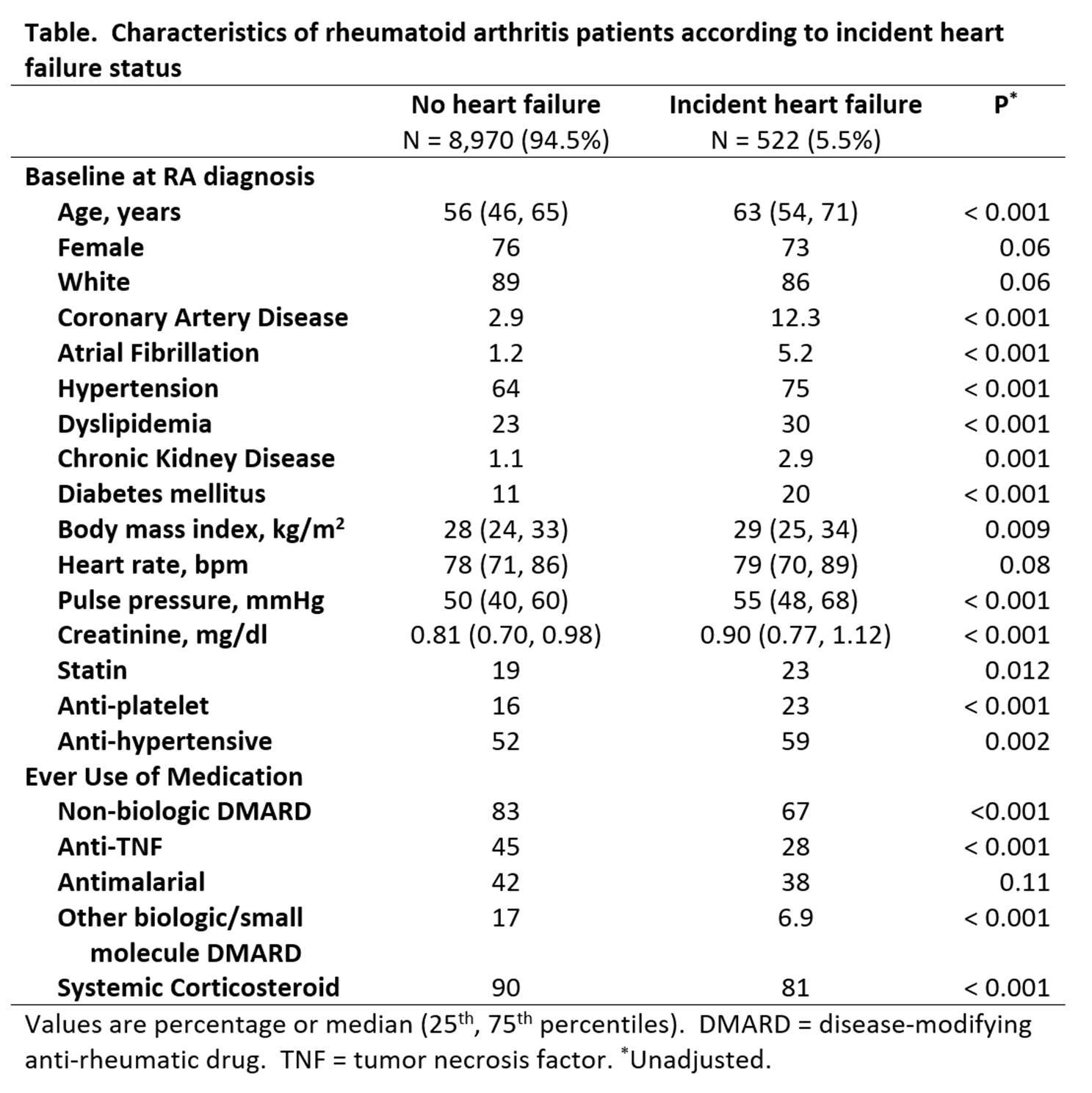
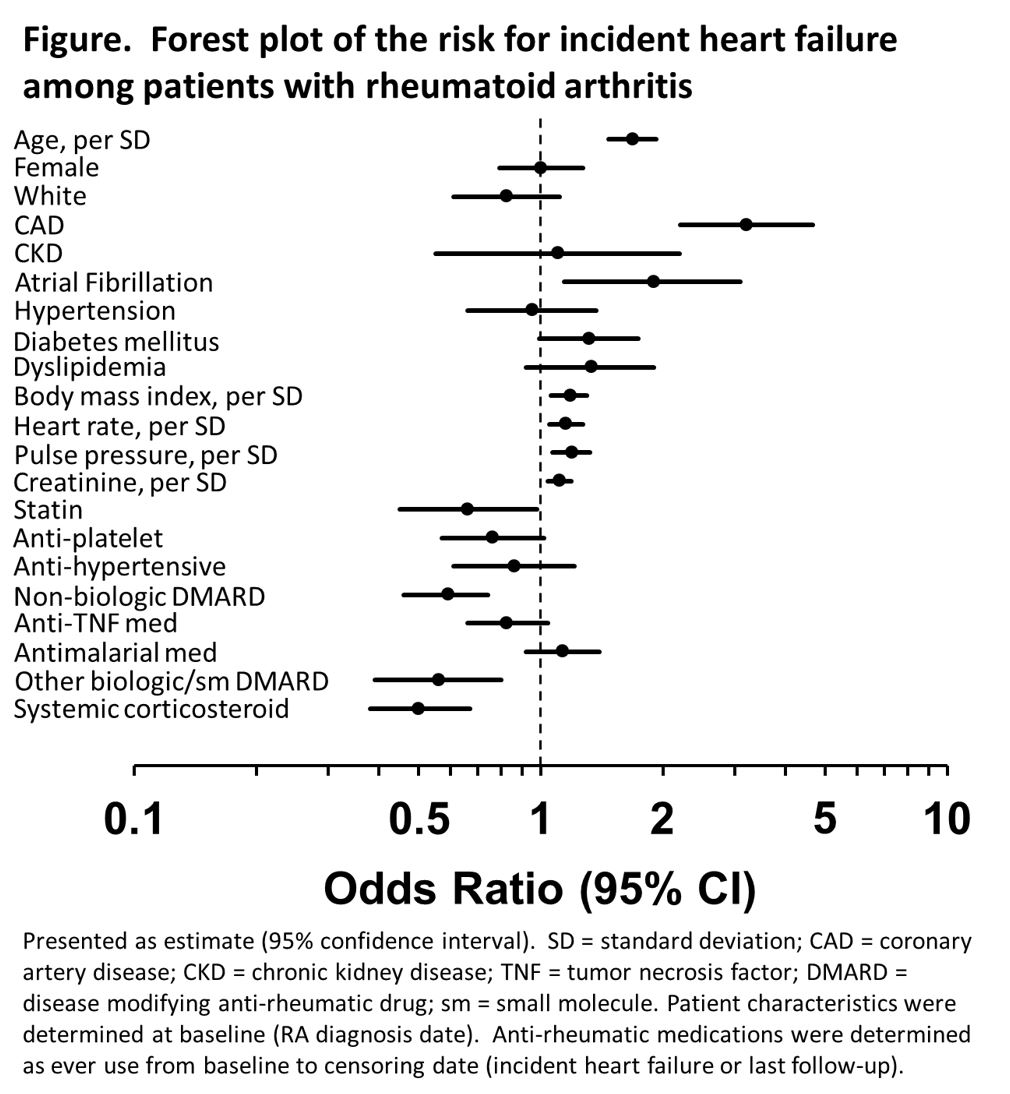
Results: Over a median 5.0 (range: 0.1 to 27) years of follow-up, a total of 522 RA patients (5.5%) developed incident HF (Table). Increasing age, CAD, atrial fibrillation, as well as higher body mass index, heart rate, pulse pressure, and creatinine at baseline (first RA ICD-9 code) were each associated with greater HF risk (Figure). The risk of HF varied by use of anti-rheumatic medication class before HF. Non-biologic DMARDs, other biologic/small molecule DMARDs, and systemic corticosteroids were associated with lower HF risk, p ≤ 0.001 for all. Anti-TNF agents and antimalarials were not associated with the risk of HF, p ≥ 0.10 for both.
Conclusion: RA patients are at risk for HF. Established cardiovascular disease or traditional risk markers are associated with increased risk. Anti-rheumatic medications variably associate with HF risk, with lower risk observed among patients taking non-biologic or other biologic/small molecule DMARDs or systemic corticosteroids.
To cite this abstract in AMA style:
Ahlers M, Stein CM, Chung CP, Ormseth MJ, Farber-Eger E, Gupta D. Heart Failure Risk Among Patients with Rheumatoid Arthritis: Association with Anti-Rheumatic Drugs [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/heart-failure-risk-among-patients-with-rheumatoid-arthritis-association-with-anti-rheumatic-drugs/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/heart-failure-risk-among-patients-with-rheumatoid-arthritis-association-with-anti-rheumatic-drugs/