Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: ANCA-associated vasculitis (AAV) leads to complications that contribute to poor quality of life and survival. Systemic vasculitis is associated with high healthcare utilization but little is known about healthcare utilization specifically in AAV, especially around the time of diagnosis when complications are common. Identifying utilization patterns is needed to define opportunities to improve care, to inform inputs for cost-effectiveness studies, and to support advocacy efforts to fund research in diseases that have a disproportionate impact on societal resources.
Methods: The Partners AAV Cohort is a consecutive inception cohort established at Partners HealthCare (PHS), a large healthcare system in New England. We included AAV cases diagnosed between 2007-2014 with available Medicare claims data who could be matched (by age, sex, and index date [AAV treatment initiation]) to a non-AAV control that received primary care at PHS and also had claims data available. Electronic health record data from cases and controls were linked deterministically to Medicare Parts A and B claims data, which contain details regarding ambulatory, inpatient, and emergency department visits and non-acute institutional visits (e.g., rehab). Healthcare utilization was compared using Chi Square tests and generalized estimating equations.
Results: We included 99 cases and controls. Age, sex, race, and baseline Charlson Comorbidity Index were similar between cases and controls (Table 1). There was an increase in emergency department (ED) and ambulatory visits (AV) and inpatient (IP) hospitalizations among AAV cases in the months preceding the index date (Figure 1). Compared to controls, cases were more likely to have at least one ED visit (67% vs 22%, P = < 0.001) and/or IP hospitalization (65% vs 15%, P= < 0.001) during the first six months following the index date (Table 1). AVs were more frequent among cases than controls throughout the study period (Figure 1, P< 0.001); in the first six months after the index date, cases had a median of 22 [13, 33] AVs compared to 5 [1, 13] among controls (Table 1). Among cases, 33% had ≥ 2 IP hospitalizations in the six months after the index date while 35% had none. Following the index date, there was a gradual decrease in healthcare utilization among cases (Figure 1). More cases than controls had ≥ 1 non-acute institutional stay (24% vs 10%, P=0.02) in the first six months after the index date (Table 1).
Conclusion: Compared to controls, AAV patients have greater healthcare utilization in the period around diagnosis. These observations establish important benchmarks in AAV care and opportunities for improvement. First, increased utilization prior to diagnosis might reflect diagnostic delays that may be shortened with strategies that include better provider education and leveraging artificial intelligence in electronic health records. Second, high utilization appears to be concentrated in a subset of AAV patients (e.g., multiple hospitalizations) which may benefit from interventions to minimize readmission or unnecessary care. Studies are needed to identify modifiable risk factors associated with healthcare utilization in AAV.
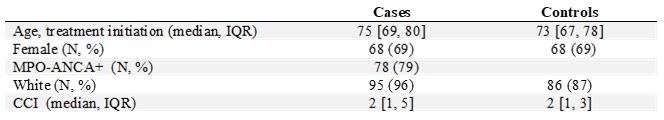 Table 1: Demographics Features of AAV Cases and Controls
Table 1: Demographics Features of AAV Cases and Controls
 Table 2: Healthcare Utilization Among AAV Cases and Controls Using Medicare Claims Data from 2007-2014
Table 2: Healthcare Utilization Among AAV Cases and Controls Using Medicare Claims Data from 2007-2014
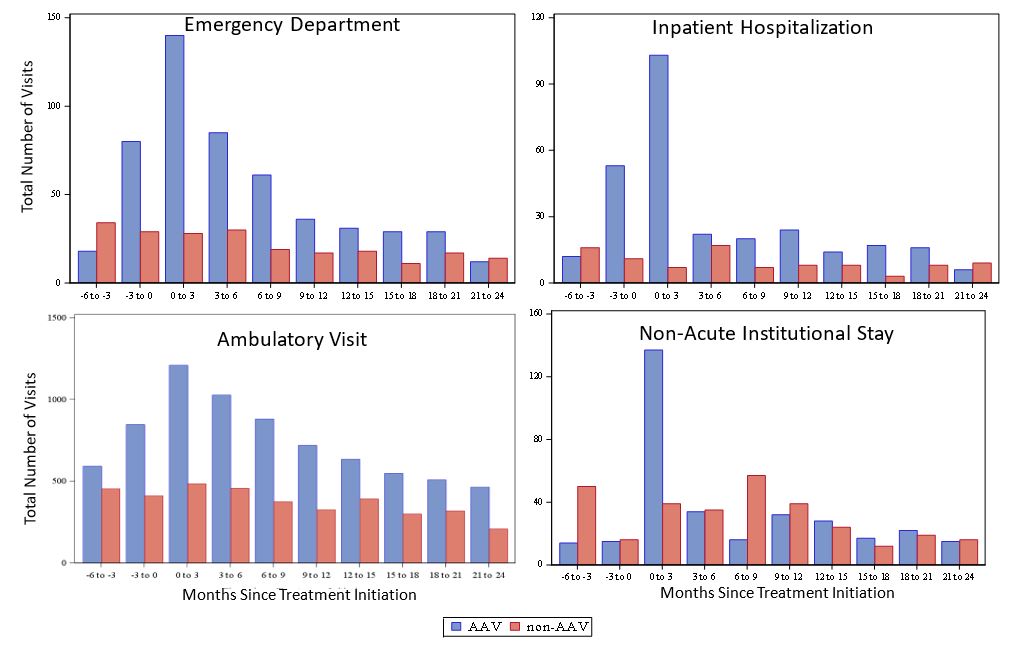 Figure 1: Healthcare Utilization in ANCA-Associated Vasculitis Before and After Treatment Initiation
Figure 1: Healthcare Utilization in ANCA-Associated Vasculitis Before and After Treatment Initiation
To cite this abstract in AMA style:
Wallace Z, Fu X, Stone J, Choi H, Walensky R. Healthcare Utilization Among Patients Diagnosed with ANCA-Associated Vasculitis Between 2007 and 2014 in a Multi-Center Cohort Linked to Medicare Claims Data [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/healthcare-utilization-among-patients-diagnosed-with-anca-associated-vasculitis-between-2007-and-2014-in-a-multi-center-cohort-linked-to-medicare-claims-data/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/healthcare-utilization-among-patients-diagnosed-with-anca-associated-vasculitis-between-2007-and-2014-in-a-multi-center-cohort-linked-to-medicare-claims-data/
