Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Guillain-Barré Syndrome (GBS) is a rare autoimmune polyneuropathy well described following viral illness, vaccination, or surgery. Systemic Lupus Erythematosus (SLE) has been associated with several neuropsychiatric syndromes including GBS. This study aims to i) Compare the risk of being hospitalized for GBS in patients with SLE compared to patients without SLE and ii) Compare the characteristics and outcomes of patients primarily admitted for GBS with and without a secondary diagnosis of SLE.
Methods: Data were abstracted from the National Inpatient Sample (NIS) Database. The numbers in the databases are weighted to optimize national estimates. The NIS 2016 and 2017 database was searched for hospitalizations of adult patients with a principal discharge diagnosis of GBS (ICD-10 code G61.0) with and without a concomitant secondary discharge diagnosis of SLE (codes M32, M32.1, M32.10, M32.11, M32.12, M32.13, M32.14, M32.15, M32.19, M32.8, and M32.9). Multivariate logistic regression model was used to calculate the adjusted odds ratio of principal discharge diagnosis of GBS and a secondary diagnosis of SLE. Age, gender and ethnicity distribution, treatment rates of plasmapheresis and IVIG, outcomes in terms of length of stay (LOS), mortality and total hospital charges were recorded and compared between the two groups. Multivariable logistic and linear regression analyses were used to adjust for confounding variables.
Results: There were over 71 million discharges documented in the combined 2016 and 2017 NIS database. A total of 16,105 hospitalizations were for adults with a principal discharge diagnosis of GBS. Of those, 130 (0.8%) had a secondary diagnosis of SLE and 15,975 (99.2%) did not have a secondary diagnosis of SLE. GBS hospitalizations with a secondary diagnosis of SLE had an adjusted odds ratio (AOR) of 2.06 (95% CI 1.35-3.12, P=0.001) compared to GBS without SLE. Characteristics of GBS patients with and without SLE are displayed in Table 1. The SLE patients were more likely to be female (88.5% vs 43.6%, p< 0.0001) and younger (44.7 vs 53.8, p=0.003). GBS with concomitant SLE was much more common in African American population compared to GBS without SLE (32% vs 8.9%, p 0.002). Total of 2,000 (12.4%) patients received PLEX. GBS with SLE patients were more likely to have received PLEX (26.9% vs 12.3%, AOR: 3.06, 95% CI 1.27-7.35, p=0.012) and had shorter length of stay (9.0 vs 11.4 days, p=0.02) in comparison to GBS patients without SLE. 3,185 (19.8%) patients received IVIG and rates of IVIG treatment were similar between the two groups (11.5% vs 19.8%, AOR: 0.48, 95% CI 0.11-2.15, p=0.338). (Table 2). From all GBS hospitalizations, 215 (1.3%) resulted in inpatient death and all of these occurred in patients without SLE.
Conclusion: Patients with SLE had 2 times the odds of being admitted for GBS compared to non-SLE patients. The inpatient prevalence of GBS in SLE in the United States was 2 cases per 1,000,000 hospitalizations. No mortality was seen in patients with GBS and SLE. Physicians should be aware of this association between SLE and GBS, and should have a high index of suspicion, when SLE patients present with neurologic manifestations suggestive of GBS.
 Table 1. Weighted descriptive characteristics of adult GBS hospitalizations with and without SLE in 2016 and 2017
Table 1. Weighted descriptive characteristics of adult GBS hospitalizations with and without SLE in 2016 and 2017
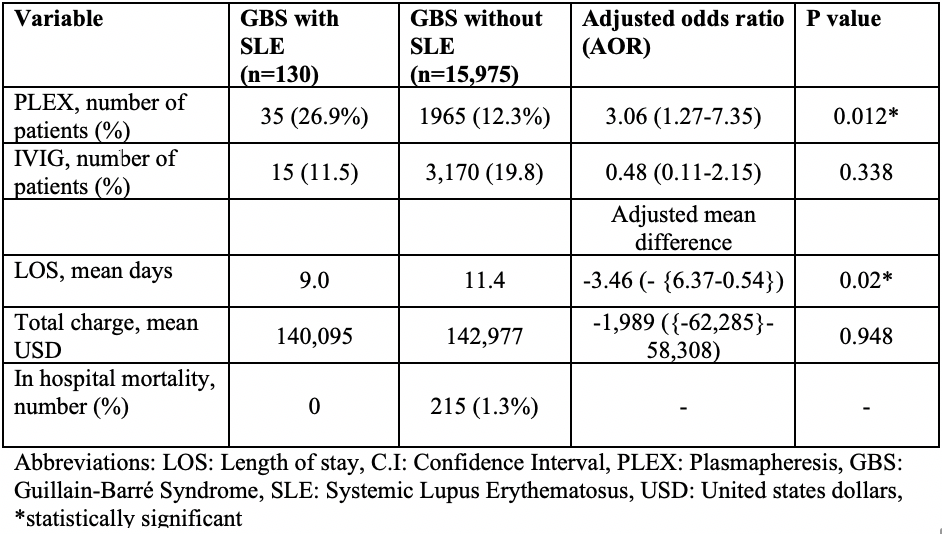 Table 2: Treatment and clinical outcomes of GBS hospitalizations with and without SLE in 2016 and 2017
Table 2: Treatment and clinical outcomes of GBS hospitalizations with and without SLE in 2016 and 2017
To cite this abstract in AMA style:
Arora S, Edigin E, Manadan A. Guillain-Barré Syndrome in Systemic Lupus Erythematosus – Results of a Nationwide Analysis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/guillain-barre-syndrome-in-systemic-lupus-erythematosus-results-of-a-nationwide-analysis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/guillain-barre-syndrome-in-systemic-lupus-erythematosus-results-of-a-nationwide-analysis/
