Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Immune checkpoint inhibitors (ICI) have greatly improved cancer outcomes but they often cause immune-related adverse vents (irAE). “Sarcoid-like” and other granulomatous reactions (GR) are an increasingly recognized irAE. The goal of this study was to analyze the range of granulomatous pathologies seen and to compare GR that occur in patients receiving anti-CTLA4, anti-PD1/PDL1, and combination anti-CTLA4/PD1.
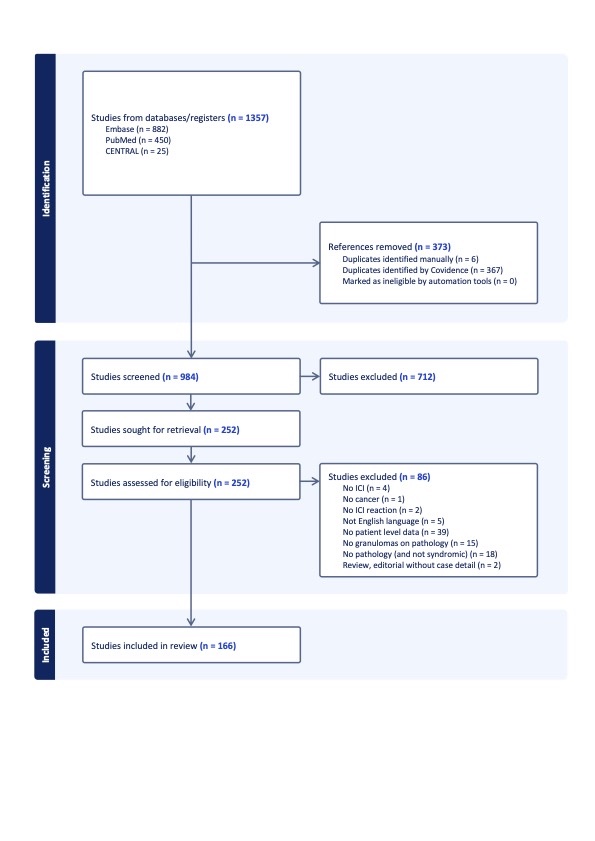
Methods: We performed a literature review of MEDLINE, Embase, and Cochrane LIbrary databases up to December 5th, 2023 to identify GR in patients treated with ICI. Inclusion criteria included documented pathology confirming a GR, or a diagnostic syndrome such as Lofgren’s or Heerfordt syndrome. Articles were independently screened for inclusion by two investigators (EW, GB) and 166 articles were included (Figure). Data was extracted including patient demographics, cancer type, ICI used, organ distribution and pathological findings. Continuous variable were compared using ANOVA and t-tests, and categorical variables compared using the chi-square test of independence.
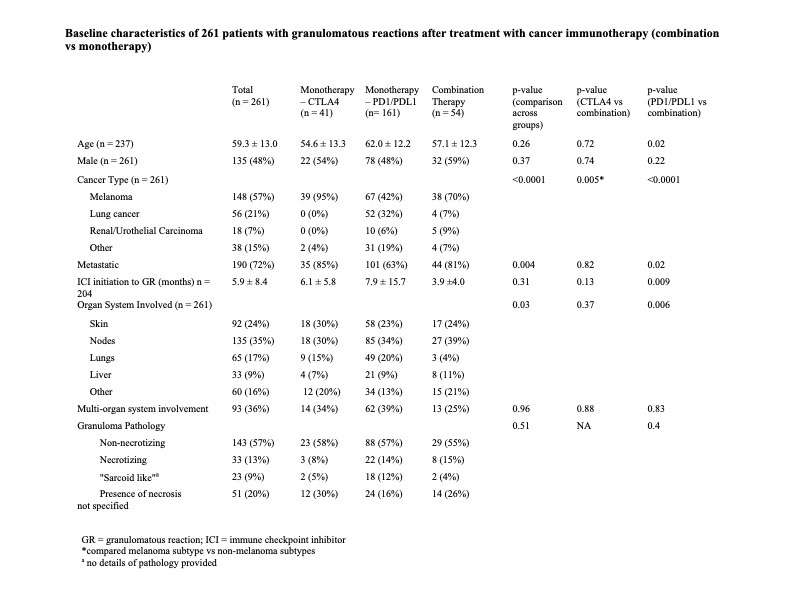
Results: A total of 261 patients were included (Table 1). The mean age at time of onset of GR was 58.3 ± 13.0 years. The most common cancer types were melanoma (57%) and lung cancer (21%). Lymph nodes (35%) and skin (24%) were the predominantly affected organs, however involvement was described in several other organs, including the liver, kidney, and bone. Single organ system involvement occurred in 64% of patients. There were no reported cases of Lofgren’s or Heerfordt syndrome.
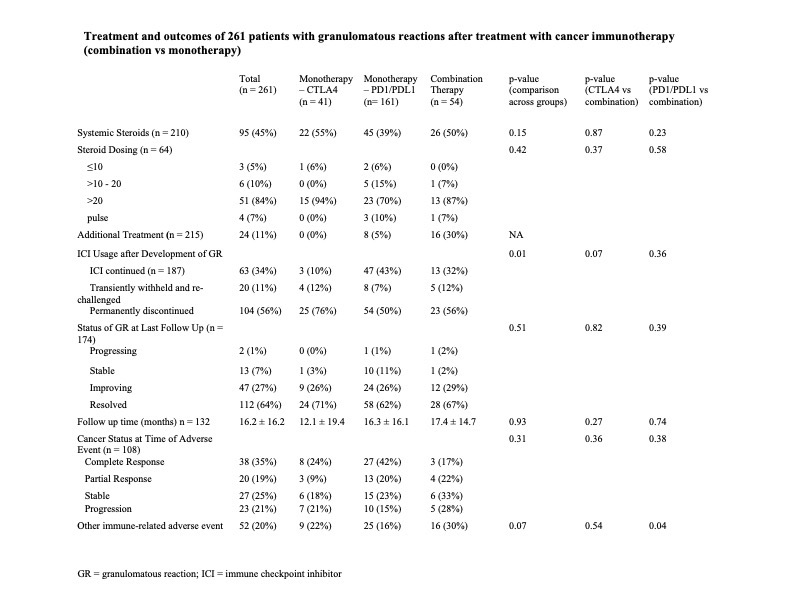
Pathology showed non-necrotizing granulomas in 57% of cases, “sarcoid-like” (no further histologic description) granulomas in 9%, and necrotizing granulomas in 13% of cases. Forty-five percent of patients were treated with systemic steroids for their GR (Table 2). 11% of patients required a steroid-sparing agent. Average follow-up time was 16.15 ± 16.19 months. Most GR (64%) had resolved by last follow-up.
Compared to those treated with combination ICI, patients treated with anti-PD1/PDL-1 monotherapy were significantly older and more likely to have lung cancer, to have a longer time to onset of the GR and to have GR involving the lungs. Patients treated with anti-CTLA4 monotherapy were largely undergoing treatment for melanoma (95%). They were more likely than those undergoing PD1/PDL-1 inhibitor and combination therapy to have treatment discontinued at time of GR. There was no difference in the frequency of necrotizing GR across the treatment groups.
Conclusion: GR in cancer patients treated with ICI can occur in many organ systems and were most commonly non-necrotizing. Patients treated with anti-PD1/PD-L1 were more likely to have GR in the lung than those treated with combination ICI. Most granulomatous reactions resolved with steroid treatment or ICI discontinuation but 11% of patients required a steroid sparing agent.
To cite this abstract in AMA style:
Wang E, Braverman G, Ghosh N, Chan K, Michot J, Bass A. Granulomatous Reactions in Cancer Patients Treated with Immune Checkpoint Inhibitors: A Systematic Literature Review [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/granulomatous-reactions-in-cancer-patients-treated-with-immune-checkpoint-inhibitors-a-systematic-literature-review/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/granulomatous-reactions-in-cancer-patients-treated-with-immune-checkpoint-inhibitors-a-systematic-literature-review/