Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Antinuclear antibodies (ANA) are biomarkers that are frequently used in the diagnosis of common autoimmune (AI) disorders, but are also present in ~12-20% of general population. Several small studies have suggested that a positive ANA test (ANA+) is associated with adverse outcomes such as cardiovascular events, cancer, and infections in the general population, but results have been inconsistent. To define the clinical consequences of ANA+, and mitigate confounding and reverse causation related with clinical testing for ANA, we used a genetic approach to test the hypothesis that a predisposition for ANA+ is associated with adverse clinical outcomes.
Methods: In BioVU, a DNA biobank linked to the de-identified electronic health record system at Vanderbilt, we studied participants of European ancestry (defined by principal components [PCs] and HapMap reference) who had genome-wide SNP genotyping performed on the Illumina Infinium MEGA® Array. We performed a genome-wide association analysis (GWAS) for ANA+ using individuals who had been tested for ANA as part of their clinical care but did not carry a diagnosis of SLE or other common AI diseases. The GWAS used an additive model, and the results were used to develop a polygenic risk score for positive ANA (PRSANA+) using Bayesian framework with continuous shrinkage. The PRSANA+ was then calculated among BioVU participants not included in the GWAS analysis. A phenome-wide association study (PheWAS) using the PRSANA+ as a predictor was performed adjusting for sex, median age, and 5 PCs of ancestry. For each condition, cases were participants having two or more phecodes for that condition and controls were those with not closely related phecode. Individuals with only one phecode for the condition were excluded. Phecodes with less than 100 cases were excluded to assure power. A false discovery rate (FDR) adjusted P-value < 0.05 was considered significant.
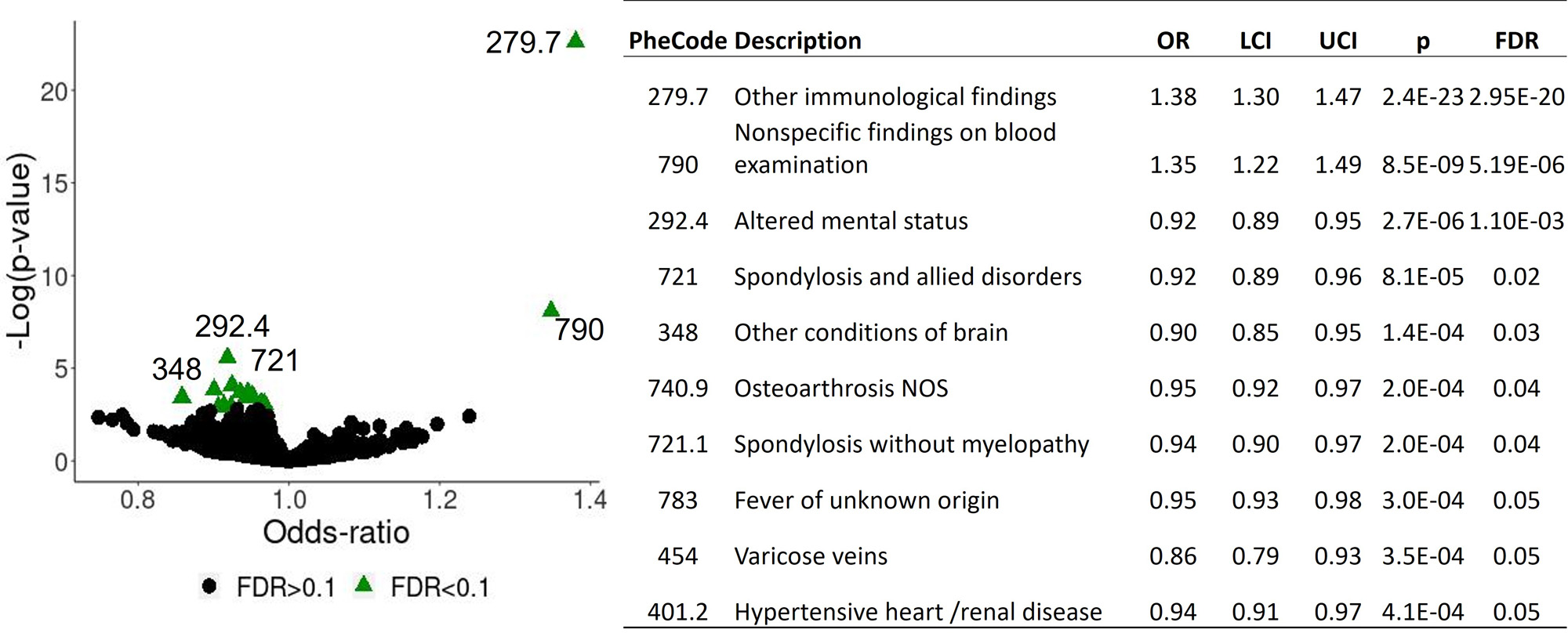
Results: There were 5,081 participants included in the GWAS, and ~7.6 million SNPs were included in the PRSANA+. The PheWAS was performed in 89,486 individuals and used 1220 phecodes. There were 10 phecodes significantly associated with the PRSANA+ at FDR≤0.05. Providing proof of concept, the top clinical associations with the PRSANA+ were phecodes related to an abnormal immunological test: “Other immunological findings” and “Nonspecific findings on blood examination” with an odds-ratio (OR)≥1.3 (P < 5.0E-05). The remaining 8 associations had an inverse association (OR < 1.0) and included neurological and back pain-related conditions, fever of unknown origin, hypertensive heart and/or renal diseases (Figure).
Conclusion: A polygenic risk score for ANA+ that captures the genetic predisposition for a positive ANA test was associated with a decreased risk for osteoarthritis, spondylosis, hypertensive renal and/heart disease, and neurological disorders. There was no evidence that a genetic predisposition to a positive ANA test was associated with an increased risk of autoimmune, cardiovascular, or other disease.
To cite this abstract in AMA style:
Karakoc G, Liu G, Zanussi J, Chung C, Gamboa J, Mosley J, Cox N, Stein C, Kawai V. Genetic Predisposition to a Positive Antinuclear Antibody Test Is Not Associated with Increased Risk of Disease [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/genetic-predisposition-to-a-positive-antinuclear-antibody-test-is-not-associated-with-increased-risk-of-disease/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/genetic-predisposition-to-a-positive-antinuclear-antibody-test-is-not-associated-with-increased-risk-of-disease/