Session Information
Date: Tuesday, November 14, 2023
Title: (2227–2256) Spondyloarthritis Including Psoriatic Arthritis – Treatment: SpA Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The impact of gender on biological and targeted synthetic therapies (ts/bDMARDs) used in PsA patients has been scarce studied. Our main objective was to explore gender differences in the incidence rate and causes of switching between ts/bDMARDs.
Methods: A retrospective longitudinal observational study was performed. Subjects: All patients who visited the outpatient rheumatology clinic from January 2007 to December 2021, and followed up to June 2022, diagnosed with PsA meeting CASPAR classification and on treatment with biological and targeted therapies (ts/bDMARDs). Main outcome: Switching of the ts/bDMARDs. Covariables: sociodemographic, clinics, and treatments. Statistical analysis: descriptive analysis of the switching, stratified by gender. To estimate ts/bDMARDs switching rates, survival techniques were used, expressing the incidence rate (IR) per 100 patients*year with their respective CI at 95% [CI 95%].
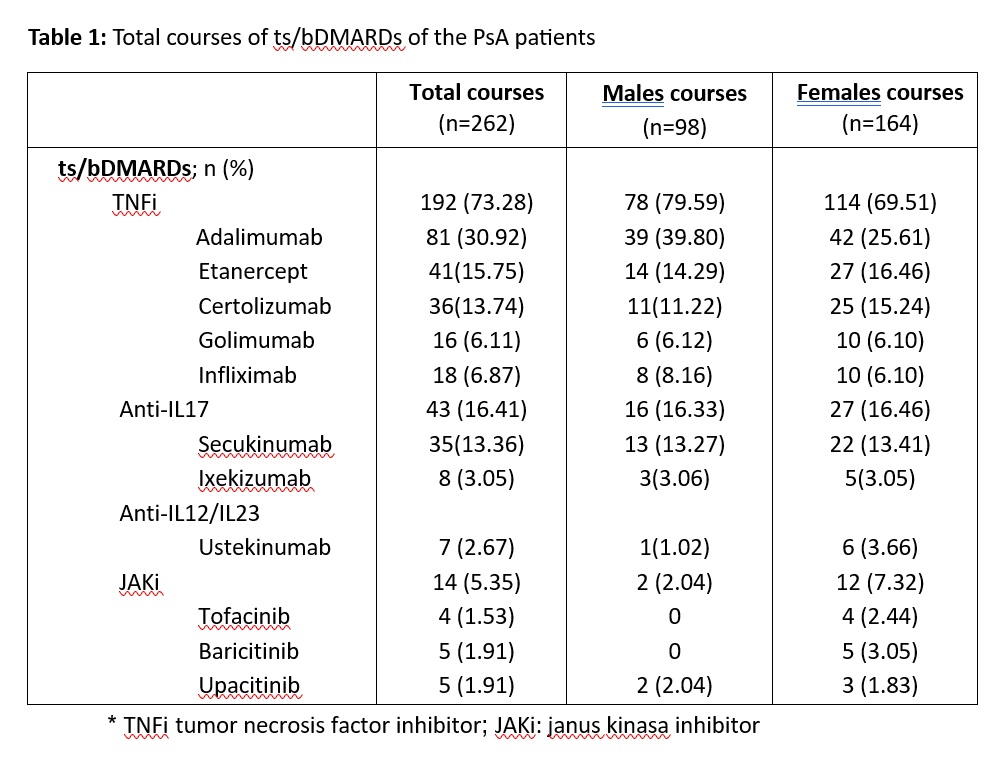
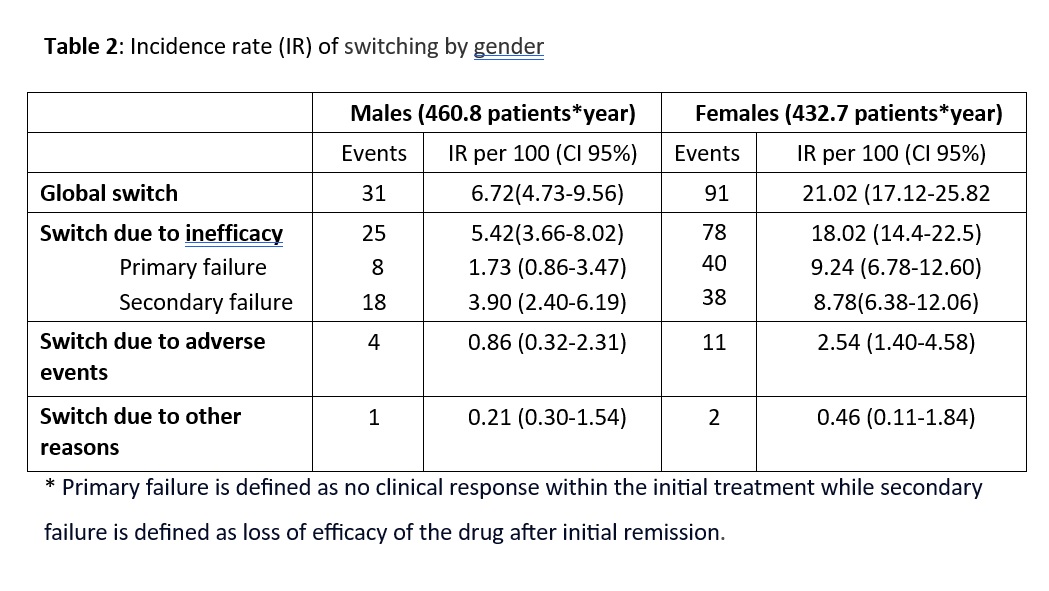
Results: A total of 141 patients with a diagnosis of PsA and under treatment with ts/bDMARDs were included, with a follow-up of 893.09 patients*year. The mean age was 48.06 ± 13.22 years and a 52.48% were females. PsA females showed some baseline disease characteristics: more depression, diabetes mellitus and thyroid disease and higher BMI. Regarding treatment characteristics, PsA males required more often concomitant corticosteroids and conventional synthetic DMARDs. A total of 262 treatment courses were recorded. Throughout follow-up, TNFi were the most used DMARDs in both genders, with 192 courses (73.28%), followed by Anti-IL17, with 43 (16.41%) courses of treatment, nevertheless, females used more Anti-IL12/23 and JAKi (Table 1). Of these 262 treatment courses, 122 (46.5%) were switched, with significative differences between gender (91 for females and 31 for males, p=0.001). About provider-reported reasons for switching, the most common reasons were primary inefficacy, loss of efficacy and adverse effects. The overall ts/bDMARDs switch rate in our study was IR (95% CI): 13.65 per 100 patients*year, with a much higher rate in females (21. 02 vs 6. 72), mainly due to primary failure. Table 2 show incidence rate (IR) of switching by gender and causes.
Conclusion: PsA female patients have distinct sociodemographic and clinic features that might contribute to the differences in therapy switching. Our results suggest that female patients are likely to change more their treatments. The overall ts/bDMARDs switch rates for females were significantly higher compared to males, mainly due to lack of efficacy. Gender differences in PsA are determined by biological and psychological factors (including gestational counselling reasons), influencing in the response to treatments and trends to switching.
To cite this abstract in AMA style:
Leon L, Freites D, Rodriguez Laguna M, Martinez C, Toledano E, Morado I, Fernandez B, Abasolo l. Gender Differences in Switching Biological and Targeted Synthetic Therapies in Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/gender-differences-in-switching-biological-and-targeted-synthetic-therapies-in-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gender-differences-in-switching-biological-and-targeted-synthetic-therapies-in-psoriatic-arthritis/