Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: To describe the GI manifestations of SLE in the RELESSER (Registry of Systemic Lupus Erythematosus Patients of the Spanish Society of Rheumatology) cohort and to determine if those are associated with a more severe disease, damage accrual and a worse prognosis.
Methods: We conducted a nationwide, retrospective, multicenter, cross-sectional cohort study of 3658 SLE patients who fulfill ≥ 4 ACR-97 criteria. Data on demographics, disease characteristics, activity (SELENA-SLEDAI), damage (SLICC/ACR/DI) and therapies were collected. Table 1 shows the different gastrointestinal manifestations among the RELESSER cohort. Demographic and clinical characteristics were compared between lupus patients with and without GI damage to establish whether GI damage is associated with a more severe disease (Table 2). χ2 tests for categorical variables and Student t-test for continuous variables were used. For non-continuous variables, either Mann-Whitney U test or logarithmic transformation were used (data expressed as median and interquartile range – IQR). Univariate linear and multivariate logistic regression analyses were performed to establish the relation of demographics, different SLE clinical manifestations, damage and GI manifestations.
Results: From 3654 lupus patients, 3.7% developed GI damage (Table 1). Patients in this group (group 1) were older (53.1 vs 46 years; p< 0.001), they had longer disease duration (16.4 vs 11.7 years; p=0.001) and were more likely to have vasculitis (14.1% vs 8.7% p=0.056), renal disease (56.1% vs 42.4% p=0.003) and serositis (40.5% vs 28.5% p=0.005) than patients without GI damage (group 2). With regard to treatment, there were statistically significant differences between both groups in terms of glucocorticoids (96.9% vs 88.6% p=0.001), azathioprine (44.2% vs 33.9% p=0.01), mycophenolate mofetil (23.7% vs 14.9% p=0.009) and cyclophosphamide (37.4% vs 21.8% p< 0.001).The use of hydroxychloroquine was more common among SLE patients with no GI manifestations related to damage (83.4% vs 75.2%, p=0.022). Hospitalizations and mortality were significantly higher in group 1 suggesting that having GI damage is linked to a worse prognosis. Moreover, patients in group 1 had higher modified SDI (2; IQR 1-4; p< 0.001) (Table 2). After the multivariable analysis, older age, high daily dose of glucocorticoids (≥ 30 mg prednisone) and higher SDI remained significant. Interestingly, even the prevalence of oral ulcers was slightly similar in both groups, the multivariable analysis revealed that the presence of oral ulcers reduced risk of developing damage in 30% of patients (Table 3).
Conclusion: Having GI damage is associated with clinical involvement of other target organs in lupus and with a worse prognosis. Patients on high dose of glucocorticoids are at higher risk of developing GI damage which reinforces the strategy of minimizing glucocorticoids. Oral ulcers are common in SLE and seem to be protective from GI damage.
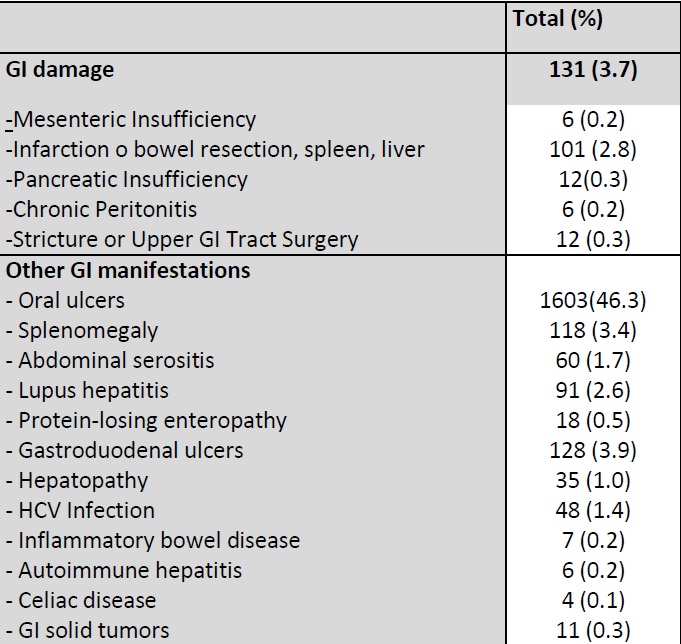 Table 1. GI manifestations in the RELESSER cohort
Table 1. GI manifestations in the RELESSER cohort
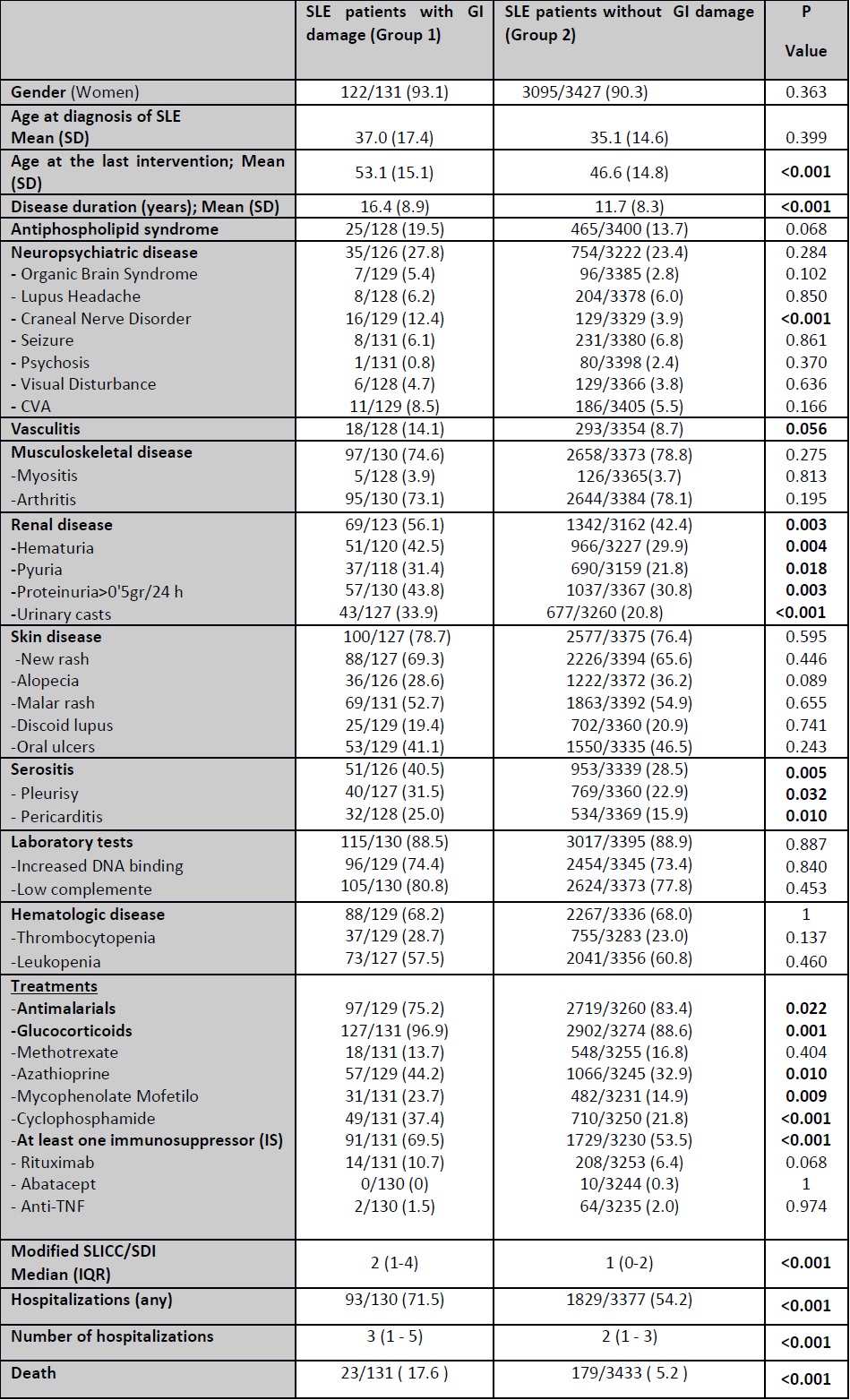 Table 2. Demographics and clinical characteristics. *Modified SLICC/SDI was calculated excluding gastrointestinal damage manifestations
Table 2. Demographics and clinical characteristics. *Modified SLICC/SDI was calculated excluding gastrointestinal damage manifestations
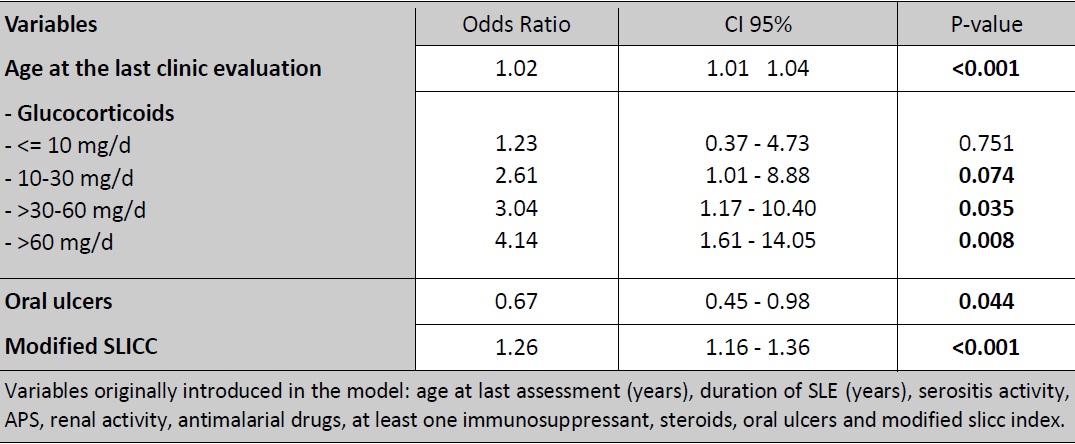 Table 3. Multivariable analysis. Variables independently associated with GI damage
Table 3. Multivariable analysis. Variables independently associated with GI damage
To cite this abstract in AMA style:
Tejera Segura B, Altabás González I, Rúa-Figueroa I, Pérez Veiga N, del Campo Pérez V, Olivé-Marqués A, Galindo-Izquierdo M, Calvo-Alén J, Ovalles-Bonilla J, Fernandez-Nebro A, Menor Almagro R, Tomero Muriel E, Del-val-del-amo N, Uriarte M, Martínez Taboada V, Andreu Sanchez J, Boteanu A, Narváez F, Morasat A, Montilla Morales C, Senabre Gallego J, Hernández Cruz B, Andrés M, Salgado Pérez E, Freire-González M, Machin Garcia S, Moriano C, Expósito L, Perez-Velasquez C, Velloso-Feijoo M, Cacheda A, Lozano Rivas N, Bonilla G, Arévalo M, Jimenez I, Quevedo-Vila V, Manero-Ruiz F, García de la Peña P, Vázquez-Rodríguez T, Ibáñez-Ruan J, Cobo-Ibañez T, Pego-Reigosa J. Gastrointestinal Disease in SLE: Does It Indicate a Worse Prognosis? [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/gastrointestinal-disease-in-sle-does-it-indicate-a-worse-prognosis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gastrointestinal-disease-in-sle-does-it-indicate-a-worse-prognosis/
