Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Although multiple national quality measures focus on the management and safety of rheumatoid arthritis, few measures address the care of patients with SLE. We used the ACR’s RISE registry to assess nationwide variations in SLE care around screening for renal disease; management of hypertension; medication safety related to prednisone and hydroxychloroquine (HCQ) use.
Methods: RISE is a national, EHR-enabled registry that passively collects data on all patients seen in participating practices, reducing the selection bias present in single-insurer claims databases. As of December 2017, RISE held validated data from 1,257 providers in 236 practices, representing ~36% of the U.S. clinical rheumatology workforce. Patients included this study were ≥18 years old and had ≥2 SLE codes ≥30 days apart between January 1 2017 and December 31 2017. Measures were assessed during this same period. We calculated 1) the proportion of patients with ≥1 documented urine study for screening for lupus nephritis (urinalysis; urine protein; or urine protein:creatinine ratio); 2) the proportion of patients with ≥2 blood pressure readings recorded ≥30 days apart; 3) the proportion of patients with systolic blood pressure >140 mm Hg or diastolic blood pressure > 90 mm Hg on ≥2 occasions, ≥30 days apart; 4) the proportion of patients prescribed ≥7.5 mg of prednisone (or equivalent) for > 90 days; 5) the proportion of patients prescribed >6.5 mg/kg of hydroxychloroquine. A practice-level analysis assessed performance on these measures among practices reporting on at least 20 patients. We also built a logistic regression model that included age, sex, race, insurance, and geographic region to assess independent predictors of performance on each measure.
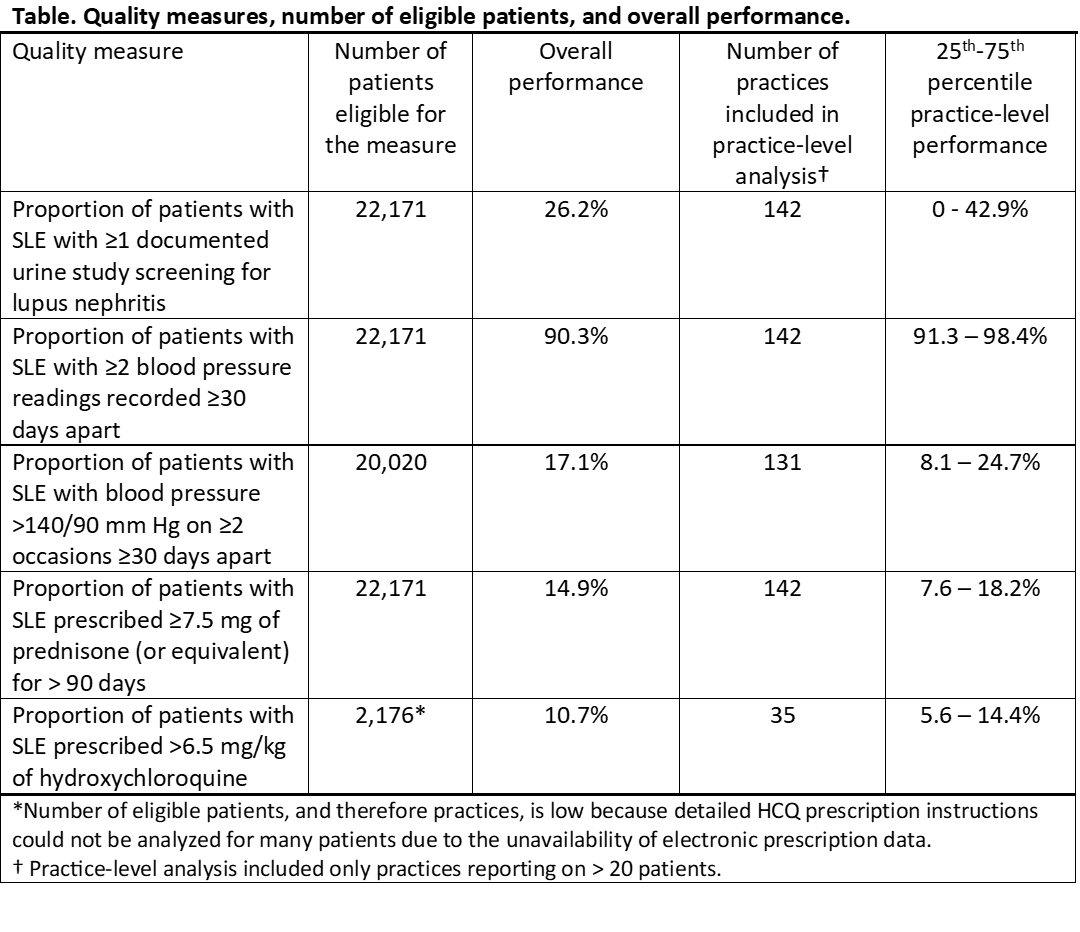
Results: We included 22,171 unique patients from 142 practices; 92% were female, 51% white, with mean age 54±15. Additional characteristics of the SLE population included that 7,485 had at least 1 documented ANA (77.7% of these with titer > 1:40); 14,751 had at least 1 dsDNA Ab (46.4% of these with titer ≥ 1:40), and 9.7% had nephritis using ICD code definitions and 0.5% had ESRD. Performance on the proposed quality measures is shown in the Table: few patients had adequate screening for lupus nephritis. Although blood pressure screening was common, a meaningful fraction had untreated hypertension. Many were receiving long-term moderate-dose steroids, or excessive doses of hydroxychloroquine. Practice and regional variation were significant. Patients who were black were more likely to have uncontrolled hypertension (OR 1.79 (1.63, 1.97)) and high prednisone dosing (OR 1.35 (1.24, 1.49)) compared to whites.
Conclusion: Significant gaps in care exist for patients with SLE across the U.S. Although some performance variation may be explained by patient factors, dramatic differences suggest that developing quality measures to address these aspects of care in SLE may improve care.
Disclaimer: This data was supported by the ACR’s RISE Registry. However, the views expressed represent those of the authors, not necessarily those of the ACR.
To cite this abstract in AMA style:
Schmajuk G, Izadi Z, Evans M, Yazdany J. Gaps in Care for Patients with SLE: Data from the ACR’s RISE Registry [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/gaps-in-care-for-patients-with-sle-data-from-the-acrs-rise-registry/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gaps-in-care-for-patients-with-sle-data-from-the-acrs-rise-registry/