Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammatory bowel disease (IBD) is an extra-articular manifestation that can appear in spondyloarthritis (SpA), as well as uveitis and psoriasis. Its prevalence is 5-10%, although subclinical intestinal inflammation has been found in up to 60%. Biological therapy(BT) can be the treatment for IBD or produce it paradoxically. Fecal calprotectin (FC) is an intestinal inflammation marker, useful for early diagnosis and monitoring disease activity.
Methods: Descriptive and retrospective study (January 2003-January 2019) of patients with SpA that develop IBD in a single center. Epidemiological variables, type of SpA, presence of IBD and its characteristics, levels of FC, presence of BT at IBD onset and treatment received were registered.
For the analysis, frequencies and percentages were used in qualitative variables and mean±standard deviation(SD) in quantitative variables. Statistical analysis was performed with IBM SPSS v.23.
Results: We studied 270 patients with SpA, 70.4% male with a mean age of 39.9±12 years. The subtypes of SpA were: ankylosing spondylitis (AS) (n=133; 49.3%), psoriatic arthritis (PsA) (n=116; 43%), undifferentiated SpA (n=16; 5.9%), SpA non-Rx axial (n=3; 1.1%) and reactive arthritis (n=2; 0.7%).
IBD was observed in 25 patients (9.26%), 80% male. At the time of IBD onset, they had a mean age of 39.12±9.8 years, the mean ESR was 31.15±24mm1ªh, CRP 2.7±2mg/dL and BASDAI 4.6. 16 patients had AS, 6 PsA and 3 undifferentiated SpA. TABLE 1.
Regarding SpA diagnosis, IBD appeared after in 15 patients with an average time of development of 8.39±8 years, before in 7 and was simultaneous in 3. The subtypes of IBD were: Crohn’s disease (CD) in 13 patients, ulcerative colitis (UC) in 9 and indeterminate colitis (IC) in 3. The FC was > 200μg/g in 17 patients (68%), normal (< 50μg/g) in 1 and between 50-200μg/g in 7. The incidence rate adjusted for follow-up of the 25 cases was 7.7 cases/1000 patients-year.
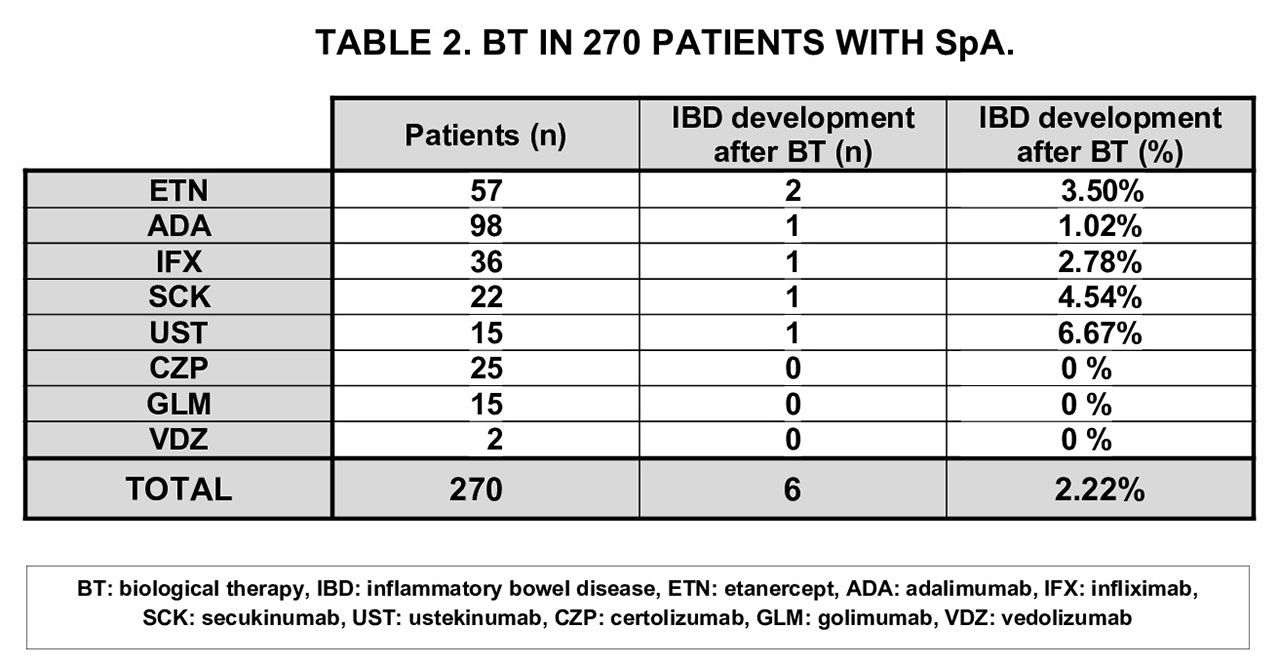
At the time of the IBD onset, 6 patients were with BT: Etanercept (ETN) (n=2), Infliximab (IFX) (n=1), Adalimumab (ADA) (n=1), Secukinumab (SCK) (n=1) and Ustekinumab (UST) (n=1). The BT had been initiated the previous 12 months in 5 of them. The incidence rate adjusted for follow-up of the 6 cases of IBD after BT was 1.83 cases/1000 patient-years. TABLE 2.
The treatment of the 25 patients with IBD was mesalazine (n=15), oral corticoid (n=5), methotrexate (n=7) and BT in all cases. The BT was: ADA (n=11; 44%), IFX (n=6; 24%), UST (n=3; 12%), golimumab (n=3; 12%), SCK (n=1; 4%) and vedolizumab (n=1; 4%). The indication was intestinal in 4 patients, joint in 8 and both in 13.
The clinical and analytical evolution in all patients was satisfactory, with a mean ESR of 11.6±9mm1ªh, CRP 0.6±0.3mg/dL and BASDAI 2 in the last control, after an average time of evolution of 12.5±9 years.
Conclusion: In our series, IBD was observed in 9.26% of patients with SpA of which 64% were AS. The most frequent form was CD and it was diagnosed after SpA in 60% of the cases. 6 patients were with BT at the time of IBD onset. High FC ( > 200μg/g) was observed in the majority of patients.
Therefore, we recommend assessing of digestive manifestations presence (abdominal pain, weight loss or diarrhea) in patients with SpA due to their possible association with IBD.
To cite this abstract in AMA style:
Calvo-Zorrilla I, García-Vivar M, Ibarguengoitia-Barrena O, Montero-Seisdedos D, Vega-Alvarez L, Blanco-Madrigal J, Fernandez-Berrizbeitia O, Ruiz-Lucea M, Torre-Salaberri I, Intxaurbe-Pellejero A, Pérez-Velasquez C, Cuende-Quintana E, Rivera-García N, Allande-López-Linares M, Ugarte-Zuazo H, Gorostiza-Hormaeche I, Galíndez-Agirregoikoa E. Frequency and Characteristics of Inflammatory Bowel Disease in Spondyloarthritis with Biological Therapy: Study of 270 Patients from the Same Center [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/frequency-and-characteristics-of-inflammatory-bowel-disease-in-spondyloarthritis-with-biological-therapy-study-of-270-patients-from-the-same-center/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frequency-and-characteristics-of-inflammatory-bowel-disease-in-spondyloarthritis-with-biological-therapy-study-of-270-patients-from-the-same-center/