Session Information
Date: Monday, November 18, 2024
Title: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Frailty represents a state of increased vulnerability to poor outcomes after physiologic stressors, and occurs at higher rates and younger ages in RA. Frailty is associated with low bone mineral density (BMD) and fractures in predominantly female RA cohorts1,2. We investigated the relationship between frailty and BMD in a predominately male cohort of Veterans with RA.
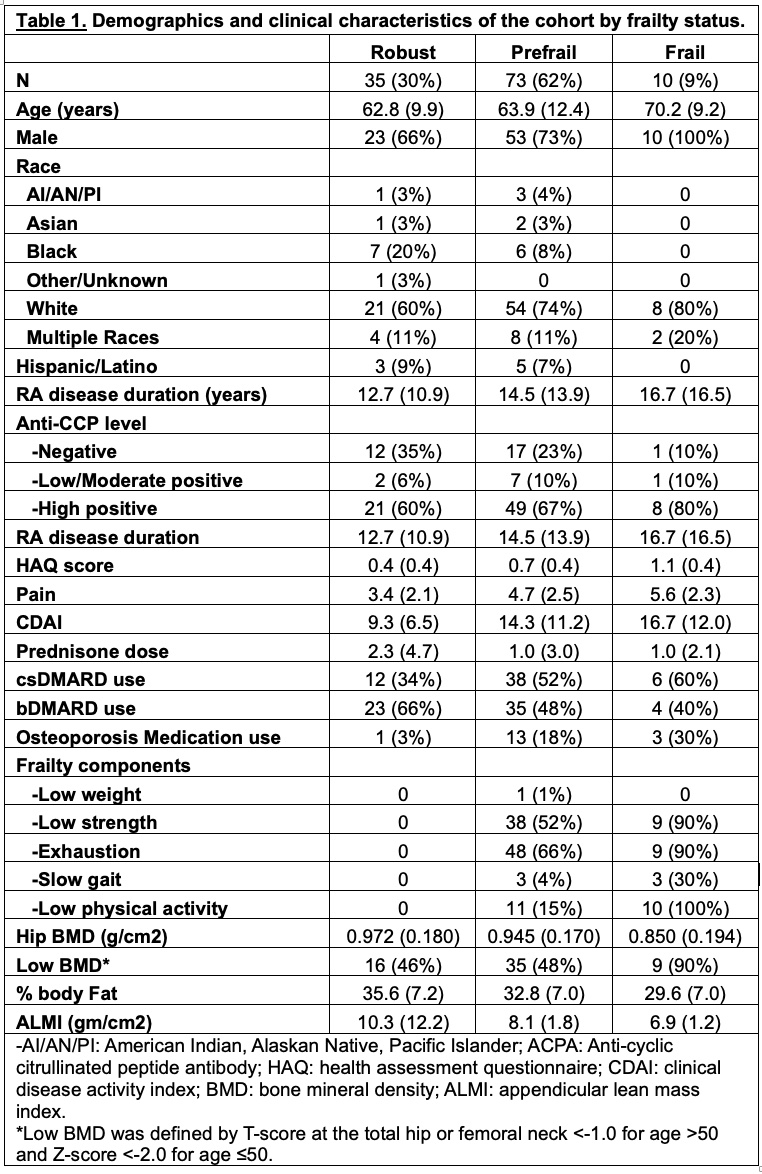
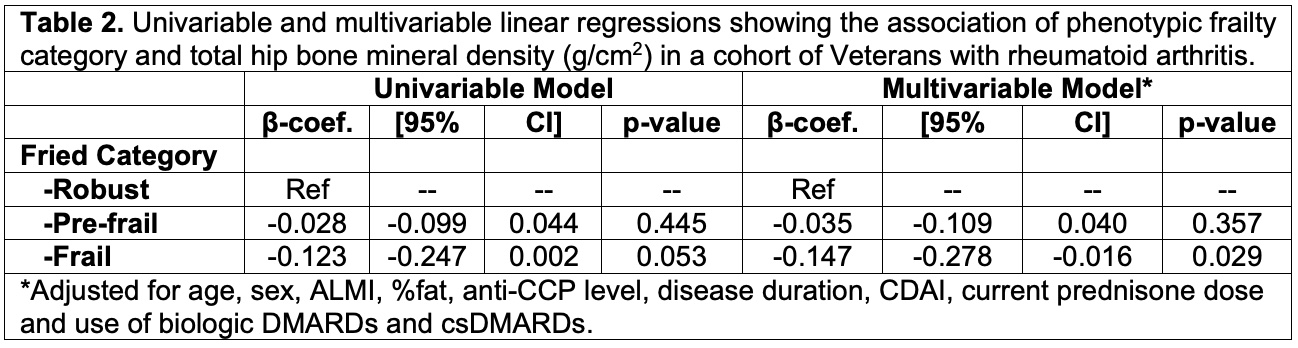
Methods: Data were from the Veterans Affairs Rheumatoid Arthritis Frailty and Osteoporosis cohort. Participants met the 2010 ACR RA classification criteria and were ≥35 years of age. Those on anabolic osteoporosis medications, androgen deprivation therapy, with hyperparathyroidism and end stage kidney disease were excluded. Frailty was measured according to the Fried Phenotype which queries 5 components – weight loss, fatigue, muscle strength, slow walking speed and low physical activity – and is categorized as robust (0 of the 5), prefrail (1-2) or frail (≥3)3. BMD and body composition (appendicular lean mass index (ALMI) and percent body fat (%fat)) were collected on a single Hologic machine using dual energy x-ray absorptiometry. Low BMD was defined by T-score at the total hip or femoral neck < -1.0 for age >50 and Z-score < -2.0 for age ≤50. Total hip BMD (THBMD) g/cm2 was our primary outcome measure. Demographics, clinical characteristics and medications were collected by self-report or the medical record. Means and frequencies were used to describe the cohort by frailty category. Univariable and multivariable linear regressions were performed to evaluate the association between frailty and THBMD controlling for age, sex, ALMI, %fat, anti-CCP level, disease duration, disease activity by CDAI, current prednisone dose and use of biologic DMARDs and csDMARDs. Osteoporosis medication use was not included in our model due to confounding by indication.
Results: 118 Veterans were included, 73% were male with a mean age of 61.411.5 years (Table 1). 70% were White, 11% Black, 12% reported multiple races, and 7% were of Hispanic/Latino ethnicity. 10 (8%) of our cohort was frail, 73 (62%) were prefrail and 35 (30%) were robust. Age, high positive ACPA, HAQ score, pain and CDAI were highest in the frail group. Prednisone dose, bDMARD use, %fat and ALMI were lowest in the frail group. The most common frailty components in the cohort were exhaustion (48%), low hand grip strength (40%) and low physical activity (18%). Low BMD was present in 90% of the frail group, 48% of the prefrail group and 46% of the robust group. In multivariable regression, we found a significant negative association between frailty and THBMD (β=-0.147 [95% CI -0.278 to -0.016], p=0.029) relative to the robust group (Table 2).
Conclusion: We found a significant association between frailty and THBMD in a predominantly male cohort of US Veterans with rheumatoid arthritis. Low BMD was prevalent throughout the cohort. Frailty measurement may identify people with RA at risk for low BMD and could be used to inform osteoporosis screening in this high-risk group. Future studies to understand if frailty predicts BMD loss are needed to support its use clinically.
1. Li G et al. Bone 2019.
2. Wysham KD et al. Bone Rep 2020
3. Fried L et al. J Gerontol A Biol Sci Med Sci 2001
To cite this abstract in AMA style:
Wysham K, Brubeck H, Riggles K, Bass R, Wahl E, Narla R, Singh N, orkaby a, Baker J, Katz P, Shoback D, Garcia J. Frailty Is Associated with Lower Bone Mineral Density in US Veterans with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/frailty-is-associated-with-lower-bone-mineral-density-in-us-veterans-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frailty-is-associated-with-lower-bone-mineral-density-in-us-veterans-with-rheumatoid-arthritis/