Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Frailty is a clinical phenotype that increases with age. However, frailty can occur in younger patients with chronic disease, including SLE. Based on few studies, frailty has been found in up to 27.5% of patients with SLE and is associated with increased mortality [1-2]. The prevalence of frailty in other cohorts of patients with SLE and its association with sarcopenia, an important related domain, or patient-centered domains, is unclear.
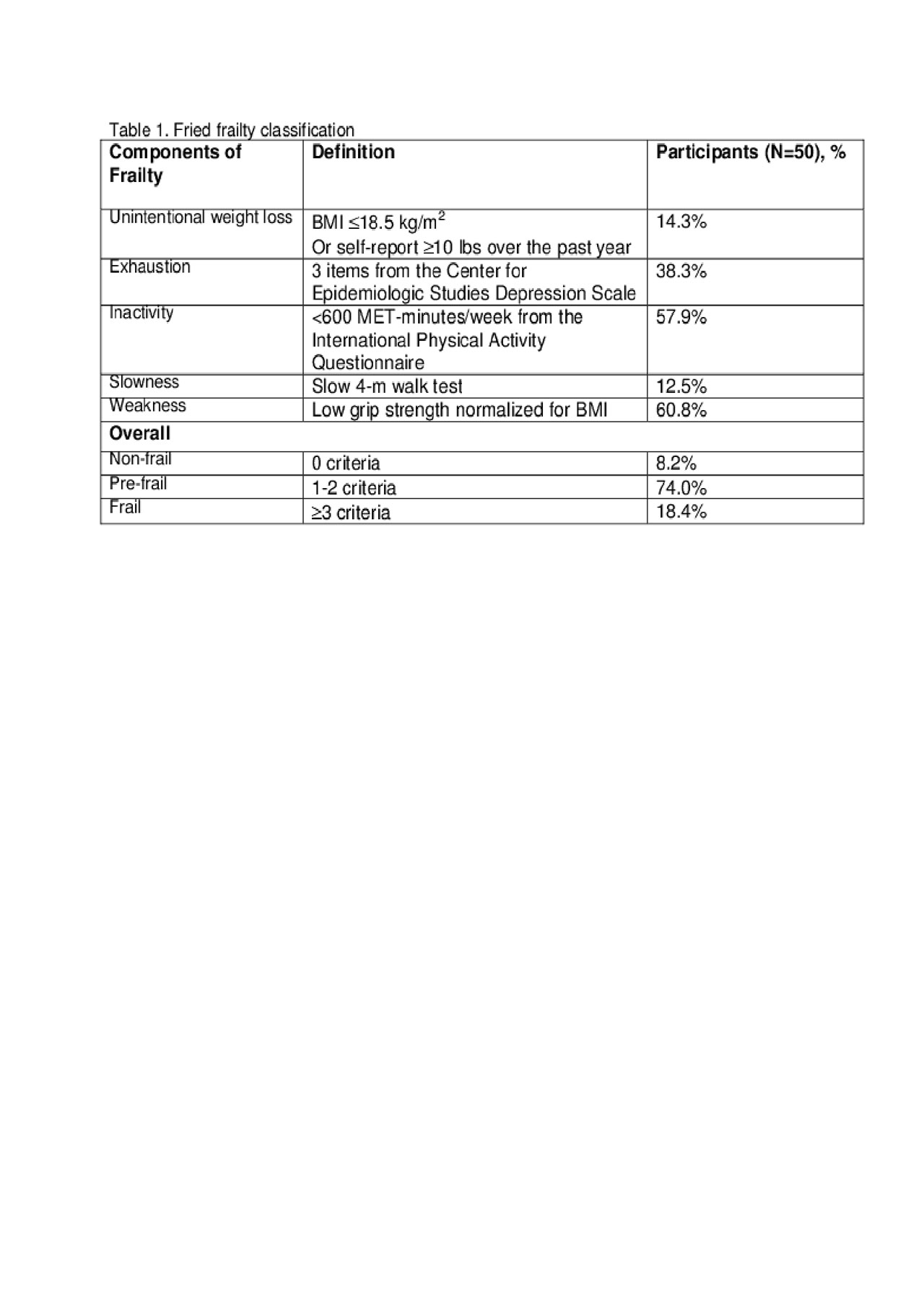
Methods: Adult women < 70 years old who fulfilled ACR criteria for SLE were recruited from a single center. Exclusions included pregnancy, dialysis, active malignancy, overlap autoimmune syndromes, or severe SLE disease activity. Frailty and pre-frailty were measured according to Fried frailty criteria [3] (Table 1). Patient-reported outcomes were measured using a) global Patient-Reported Outcomes Measurement Information System (PROMIS) computerized adaptive tests and b) the disease-specific LupusQOL. Disease activity was measured with the SELENA-SLEDAI, and damage with the SLICC/ACR index. DXA was used to compute sarcopenia [4] (Table 2). Differences between frail, pre-frail, and non-frail participants were evaluated using chi-square tests and Kruskal-Wallis tests as appropriate.
Results: 50 women enrolled from 8/2018-3/2019. Although median age was only 51 years, 74% and 18% were pre-frail and frail, respectively (Table 1). Frail women had increased disease activity and damage as compared to pre-frail and non-frail women; however, this did not differ significantly across the three groups (Table 2). Age and comorbidities, including fibromyalgia, were similar between non-frail, pre-frail, and frail women. Educational attainment differed significantly across pre-frail, frail and non-frail patients (p=.03), with a larger proportion of lower educational attainment among frail women. Significant differences in PROMIS mobility (p=0.004), physical function (p=0.014), pain interference (p=0.030), and fatigue (p=0.004) and LupusQOL physical health (p=0.008) and pain (p=0.008) were observed across frailty groups, with frail women reporting clinically meaningfully worse scores in all measures. While not statistically significantly different across the frailty groups, frail women were 6x more likely to be sarcopenic (Table 2).
Conclusion: The prevalence of frailty and pre-frailty is high in this cohort of mid-aged women with SLE. Frailty did not appear to be a proxy for comorbidity or fibromyalgia. Compared to pre-frail and non-frail women, frail women had poorer health-related quality of life and a higher proportion of sarcopenia. Data collection is ongoing to clarify the relationship between frailly and potential confounders. If frailty is associated with worse health outcomes, it could be a potential therapeutic target.
1. Katz et al. 2017
2. Legge et al. 2019
3. Bandeen-Roche et al. 2006
4. Cruz-Jentoft et al. 2019
To cite this abstract in AMA style:
Lieber S, Paget S, Berman J, Barbhaiya M, Sammaritano L, Kirou K, Carrino J, Sheira D, Finik J, Mandl L. Frailty and Sarcopenia in Women with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/frailty-and-sarcopenia-in-women-with-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frailty-and-sarcopenia-in-women-with-systemic-lupus-erythematosus/