Session Information
Date: Tuesday, November 15, 2016
Title: Muscle Biology, Myositis and Myopathies - Poster II: Clinical
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Due to the rarity of the entity, the literature on focal myositis (FM) fails to address important questions on its nosology, associated disorders, clinical presentation and therapeutic management. We sought to shed light on clinical, pathological, and therapeutic features of FM through the analysis of data from a large patient cohort.
Methods: We searched for confirmed cases of FM in the Lyon University Hospital’s database of patients diagnosed with myositis since year 2000. FM was diagnosed as per the usual clinicopathological definition. Clinical, serological, imaging, pathological and therapeutic data were collected. When missing from the original pathological analysis, complementary immunohistochemistry was redone when possible.
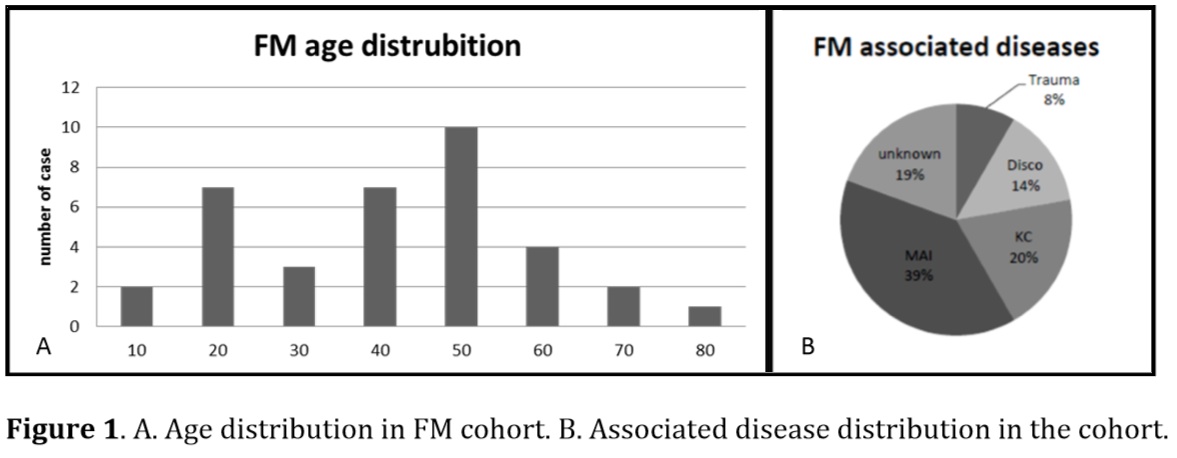
Results: Of the 810 patients included in the myositis database, 36 (4.4%) had confirmed FM (22 males, 14 females, mean age=45) (Figure 1.A). The main clinical signs were focal muscular pain (78%), fever (28%) and local erythema (36%). Serum creatine kinase was usually normal (81%); conversely, serum immunological abnormalities (mild to marked inflammation as determined by ESR or CRP, autoantibodies such as anti nuclear or anti-extractable nuclear antigen, and dysglobulinemia) were found in the sera of 58% of the patients. Beyond confirming previously-reported findings, the pathological analyses also illustrated significant rates of vascularitis within the muscle (73%) and fasciitis (75%). While FM’s etiopathogeny remains enigmatic, this study highlighted frequent association with immune-mediated inflammatory disease (IMID) (39%), neoplasia (19%), radiculopathy (14%) and trauma (8%) (Figure 1.B). IMID included Behcet’s disease (n=5), various inflammatory rheumatic diseases (n= 5) and others. Neoplasms were solid cancers in six cases (bladder n=2, thyroid n=1, skin n=1, prostate n=1, and adenocarcinoma of unknown primary site n=1), and hemopathies in two (one had both). Contrasting with the usual perception, two-thirds of the cohort required immunosuppressive therapy. As first line, all patients received steroids. The recurrence rate was 36%. In case of refractory disease, or frequent relapses, a second line was considered with azathioprine, methotrexate, intravenous immunoglobulin or cyclophosphamide. Interestingly, when underlying disease was present, the FM clinical course was often correlated with the associated pathology evolution.
Conclusion: This study provides new clinic-pathological features to define FM. Despite of the classic view of a seldom painful and spontaneously resolving disorder, this work suggests that FM can be a serious disease and require active treatment. Moreover, these results suggest that FM patients should receive IMID and neoplasia screening.
To cite this abstract in AMA style:
Gallay L, Petiot P, Hot A, Thivolet-Bejui F, Streichenberger N. Focal Myositis: New Insights on Diagnosis and Pathology [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/focal-myositis-new-insights-on-diagnosis-and-pathology/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/focal-myositis-new-insights-on-diagnosis-and-pathology/