Session Information
Date: Monday, October 27, 2025
Title: Abstracts: Rheumatoid Arthritis – Treatment I: Preventative and Novel Treatments (1674–1679)
Session Type: Abstract Session
Session Time: 1:45PM-2:00PM
Background/Purpose: While conventional synthetic DMARDs (csDMARDs) remain first line therapy in early RA, most patients do not achieve sustained remission, and a subgroup develop difficult-to-treat RA (D2TRA). More effective remission induction is achieved with first line biologic DMARDs (bDMARDs), which have a comparable safety profile to csDMARDs in clinical trials. Falling treatment costs through biosimilar use further support the health economic argument for first line bDMARD, particularly for anti-TNF drugs. Beyond early remission induction, it is important to assess whether first-line bDMARDs improve long-term outcomes compared with csDMARD treat-to-target approach.
Methods: An Inflammatory Arthritis cohort was used to identify DMARD-naive early RA patients treated with an anti-TNF as first-line induction therapy for 12 months as part of a clinical trial. Early RA patients who received usual care with treat-to-target csDMARDs were used as controls. All patients had ≥5 years follow-up. Outcomes at 5 and 10 years were categorized as: 1) drug free remission, 2) csDMARDs only, 3) single bDMARD, 4) failure of bDMARD class or 5) failure of ≥2 mechanisms of actions (MoA) of b/tsDMARDs (EULAR D2TRA criterion #1 [1]). Rates of sustained remission (DAS28 or clinician-documented remission for ≥6 months) and time to first bDMARD were evaluated. Analyses used multinomial and binary logistic regression and Wilcoxon rank-sum test.
Results: 114 anti-TNF induction patients and 228 matched controls with RA, diagnosed between 2007-2015, were included. Baseline characteristics were similar between groups (Table 1). All cases that satisfied “failure of ≥2 MoA b/tsDMARDs” also fulfilled all three criteria of the EULAR definition for D2TRA. At 5 years, only 0.9% were D2T in the anti-TNF group compared to 7% in the controls (OR 0.11, p=0.033) (Table 2). Rates of drug free remission were also significantly higher in the anti-TNF group compared to the controls at 5 years (13.2% vs 6.1%, OR 2.25, p=0.049). Eighty-eight percent of all patients had 10-year follow-up data available. The differences in rates of D2TRA and drug free remission at 10 years were no longer apparent. However, a significantly higher proportion of patients who received anti-TNF induction therapy were on single bDMARD at 10 years compared to the csDMARD controls (27.7% vs 12.5%, OR 2.64, p=0.006). Sustained remission was more frequent in the anti-TNF group compared with controls at 10 years (62% vs 45%, adjusted OR 1.91, p=0.014). The median adjusted time to require escalation to biologic therapy was 52.5 months in the anti-TNF group compared to 39.3 months in the control group (p=0.019).
Conclusion: These data suggest first line anti-TNF induction therapy in RA is associated with better long-term outcomes compared with treat-to-target csDMARD approach with favourable health economic data. Fewer than 1% of anti-TNF treated patients were D2T at 5 years. Furthermore, fewer anti-TNF treated patients required ≥2 bDMARDs at 10 years and a higher proportion achieved sustained remission. This real-world study further highlights the potential benefits, including costs, to be realised from adopting routine first line bDMARD use in early RA.
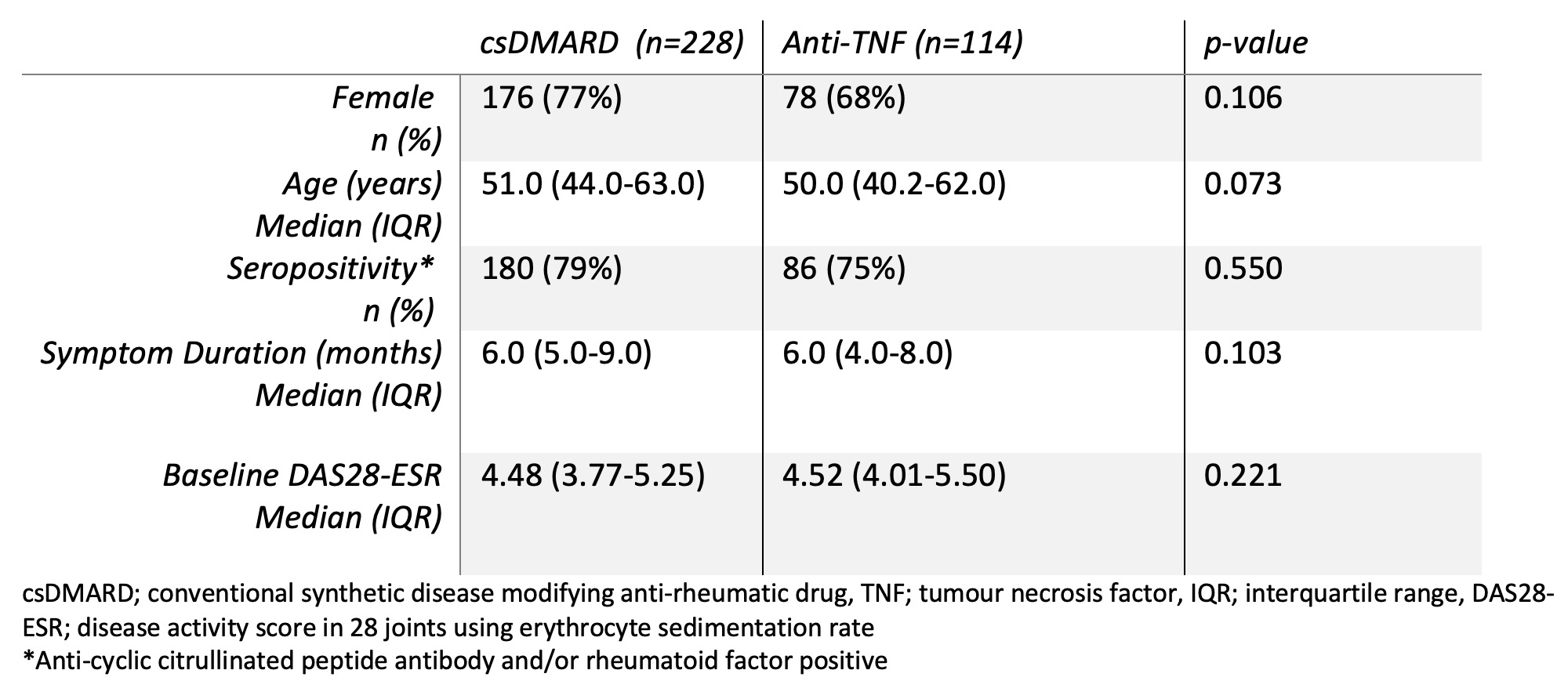 Table 1. Baseline characteristics
Table 1. Baseline characteristics
.jpg) Table 2. Clinical outcomes at 5 and 10 years
Table 2. Clinical outcomes at 5 and 10 years
To cite this abstract in AMA style:
Toyoda T, Abacar K, Shuweihdi F, Sheridan M, Nam J, Tan A, Bissell L, Emery P, Mankia K. First line anti-TNF therapy in early rheumatoid arthritis is associated with a lower frequency of difficult-to-treat disease at five years and better long-term outcomes compared with usual care [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/first-line-anti-tnf-therapy-in-early-rheumatoid-arthritis-is-associated-with-a-lower-frequency-of-difficult-to-treat-disease-at-five-years-and-better-long-term-outcomes-compared-with-usual-care/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/first-line-anti-tnf-therapy-in-early-rheumatoid-arthritis-is-associated-with-a-lower-frequency-of-difficult-to-treat-disease-at-five-years-and-better-long-term-outcomes-compared-with-usual-care/
