Session Information
Session Type: Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Primary systemic vasculitis (PSV) patients on immunosuppression are at higher risk of adverse outcomes following COVID-19 infection and often mount suboptimal vaccine responses to SARS-CoV-2 vaccination. The aim of this study was to investigate risk factors for first breakthrough COVID-19 infection after two vaccine doses in this patient group, from 02 January 2021 to 01 April 2023.
Methods: PSV patients enrolled in a prospective, UK-based multicentre observational cohort study investigating serological responses to SARS-CoV-2 vaccination (ethics reference: 20/EM/0180) were included if they had two SARS-CoV-2 vaccine doses. Patients were excluded if they had a previous history of documented COVID-19 infection or if their SARS-CoV-2 anti-nucleocapsid antibody titre (anti-N IgG) was >6104 median fluorescence intensity (MFI) indicating previous infection1. First symptomatic breakthrough SARS-CoV-2 infection (PCR or lateral flow positive) >14 days after a second SARS-CoV-2 vaccination was the outcome of interest. SARS-CoV-2 IgG spike antibody (anti-S IgG) and anti-N IgG titres were measured using a Luminex assay, and seroconversion was defined as an anti-S IgG titre >1896 MFI1. Clinical details were obtained via electronic health records.
1Smith et al. BMC Nephrol. 2022 May 31;23(1):199
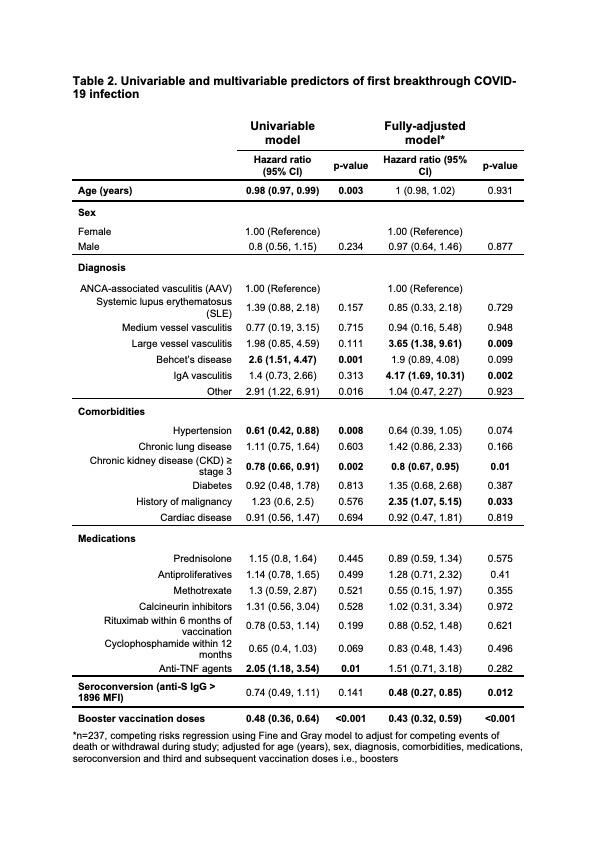
Results: 252 PSV patients were identified, with 13 of these excluded (n = 9 had COVID-19 prior to or within 14 days of their second vaccination, n = 4 withdrew consent), leaving 239 eligible patients (48.5% male, median age 58.8 years) for the analysis, mainly consisting of ANCA-associated vasculitis (AAV) patients (Table 1). Median follow-up was 400 (range 78–756) days. During follow-up, 117 patients (49.0%) had a first breakthrough COVID-19 infection, representing a crude incidence rate of 12.0 per 10,000 person-days. 14 required inpatient admission (12.0%), with two being admitted to intensive care. One patient died of COVID-19. Median time from second vaccination to first breakthrough infection was 350 (interquartile range 285–442) days. Univariable and multivariable analyses of first breakthrough infection were conducted using the Fine and Gray method to adjust for the competing events of death and study withdrawal. In the fully-adjusted model, seroconversion and third and subsequent vaccinations i.e., boosters were associated with a lower hazard of breakthrough infection, with hazard ratios of 0.48 (95% confidence interval [CI] 0.27–0.85; p=0.012) and 0.43 (95% CI 0.32–0.59; p< 0.001) respectively. Chronic kidney disease was also associated with reduced hazard in fully-adjusted analysis (p=0.01). Patients with a history of malignancy (p=0.033), and those with IgA vasculitis and large vessel vasculitis (relative to AAV) were all at higher hazard for breakthrough infection (p=0.002, and p=0.009 respectively, Table 2)
Conclusion: In this cohort of PSV patients on immunosuppression who had two SARS-CoV-2 vaccinations, a third and subsequent vaccine doses were independently associated with reduced risk of breakthrough COVID-19 infection. Our study highlights the importance of booster vaccinations and support anti-S IgG titres as a correlate of protection against COVID-19 in this group of patients.
To cite this abstract in AMA style:
Chen-Xu M, Cooper D, Döffinger R, Jones D, Smith R. First Breakthrough COVID-19 Infection Following Two SARS-CoV-2 Vaccinations Among Primary Systemic Vasculitis Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/first-breakthrough-covid-19-infection-following-two-sars-cov-2-vaccinations-among-primary-systemic-vasculitis-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/first-breakthrough-covid-19-infection-following-two-sars-cov-2-vaccinations-among-primary-systemic-vasculitis-patients/