Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Fibromyalgia is a non-autoimmune disease with widespread pain, severe fatigue, and sleep problems. There are limited studies examining the association between fibromyalgia and autoimmune conditions, and so far, there is no evidence showing that fibromyalgia could be a potential initial presentation for autoimmune diseases. We aim to investigate the potential association between fibromyalgia and autoimmune conditions.
Methods: We conducted a retrospective, propensity score matched study using the TriNetX database, a network comprising deidentified data across the world. We included 14,309 patients who were diagnosed with fibromyalgia between November 1, 2018, and January 1, 2019, from 118 health institutions worldwide with no existing diagnosis of autoimmune conditions before or up to 1 month after the diagnosis of fibromyalgia, comparing them with a matched control group without fibromyalgia diagnosis. The primary outcomes were development of autoimmune conditions and number of ambulatory visits between 1 month and 5 years after the diagnosis of fibromyalgia. Propensity score was matched by incorporating variables including age, gender, race, smoking history, family of arthritis and other connective tissue diseases, body mass index (BMI).
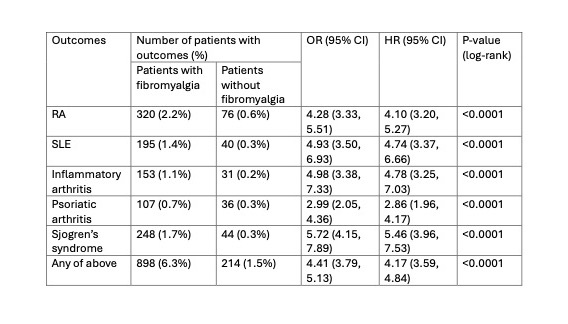
Results: The median age was 57 ± 15 years, with 91% females, and 84% white individuals in both groups. In our risk assessment, 320 (2.2%) out of 14,309 patients diagnosed with fibromyalgia developed rheumatoid arthritis (RA) in the next 5 years compared to 76 (0.5%) in the control group without fibromyalgia (odds ratio (OR), 4.28, 95% confidence interval (CI), [3.33, 5.51]). In Kaplan – Meier survival analysis, fibromyalgia was found to be associated with higher risk of developing RA (hazard ratio (HR), 4.10, 95% CI, [3.20, 5.27], p< 0.0001). There were 195 (1.4%) patients developing systemic lupus erythematous (SLE) in fibromyalgia group compared with 40 (0.3%) patients in control group (OR, 4.93, 95% CI, [3.50, 6.93]). In Kaplan – Meier analysis, fibromyalgia was associated with higher risk of SLE (HR, 4.74, 95% CI, [3.37, 6.66]). Similarly, fibromyalgia was found to be associated with higher incidence of Sjogren’s syndrome, psoriatic arthritis, and inflammatory arthritis (table 1). Patients with fibromyalgia also tend to have more ambulatory visits in the next 5 years compared with control group (76 vs 45, p < 0.0001).
Conclusion: Overall, fibromyalgia is associated with higher risk of autoimmune conditions and could be a potential initial manifestation of autoimmune conditions. As providers, we should be alarmed if our patients start to show signs of arthralgia or other signs of autoimmune disorders instead of attributing everything to fibromyalgia. Further studies are needed to evaluate potential predictors for future development of autoimmune conditions in fibromyalgia patients.
To cite this abstract in AMA style:
Wang Q, Chaudhary P, Chang Y, Garg M. Fibromyalgia as a Potential Initial Presentation for Autoimmune Conditions [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/fibromyalgia-as-a-potential-initial-presentation-for-autoimmune-conditions/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/fibromyalgia-as-a-potential-initial-presentation-for-autoimmune-conditions/