Session Information
Date: Monday, November 18, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Psoriatic arthritis (PsA) is a chronic immune-mediated inflammatory disease of the joints, affecting up to a third of individuals with cutaneous psoriasis. Pathogenesis remains insufficiently understood, and is likely a combination of environmental triggers, genetic predisposition, and immune pathway/s activation. Prior research suggests that up to 40% of patients with PsA have a family history of psoriatic disease (i.e., psoriasis [PsO] and/or PsA). However, it is unclear whether this family history contributes to either a distinct PsA phenotype and/or timing of disease onset. We aimed to identify differences in presentation, domain involvement, and disease activity between those with and without first-degree relatives (FDR) with psoriatic disease.
Methods: 793 patients meeting CASPAR criteria for PsA were enrolled into a prospective, longitudinal database (NYU Psoriatic Arthritis Cohort; PAC). Demographics, medical history, family history, as well as psoriatic disease phenotype and disease activity were recorded. The effects of psoriatic disease family history on PsA was investigated via independent sample t-tests, chi-square tests, and ANOVA as appropriate.
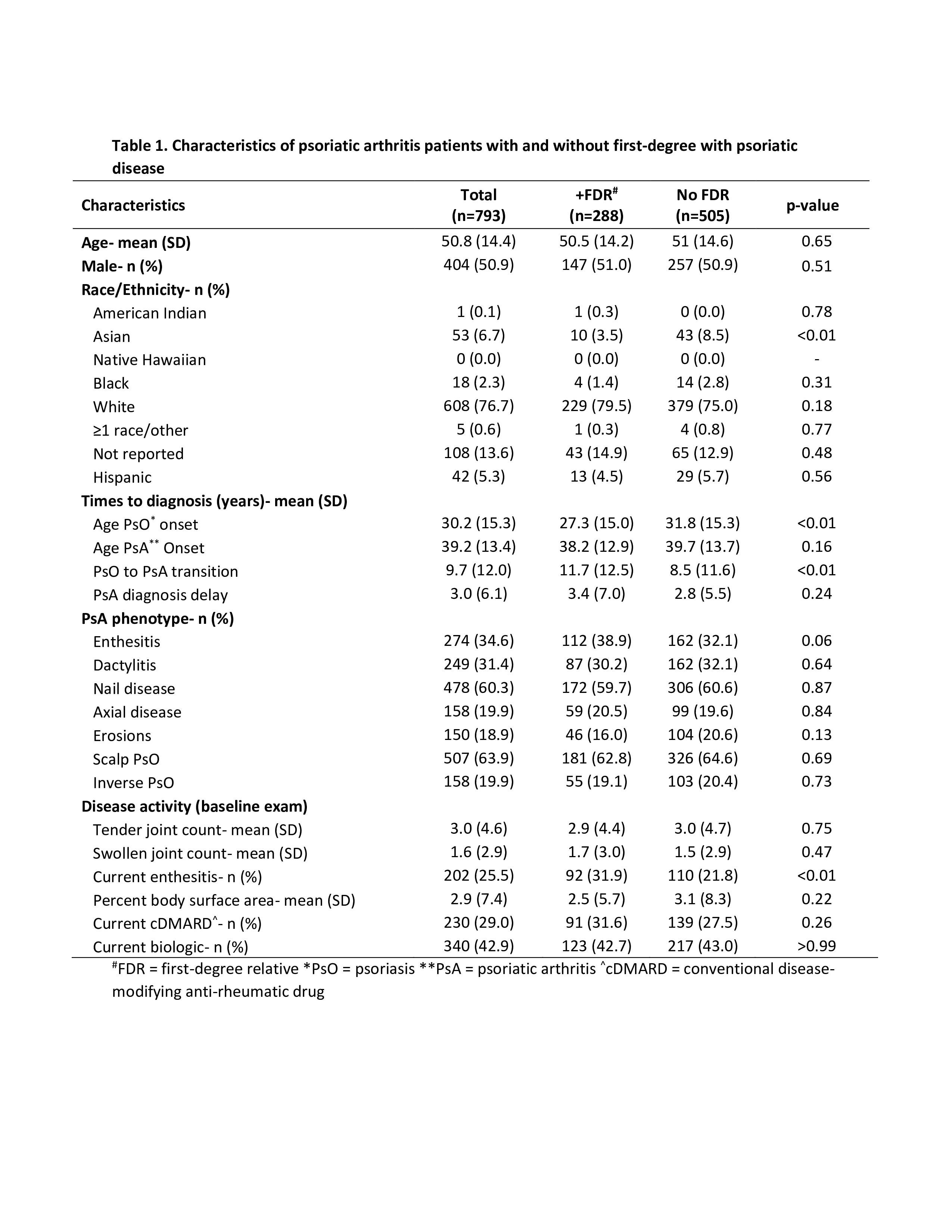
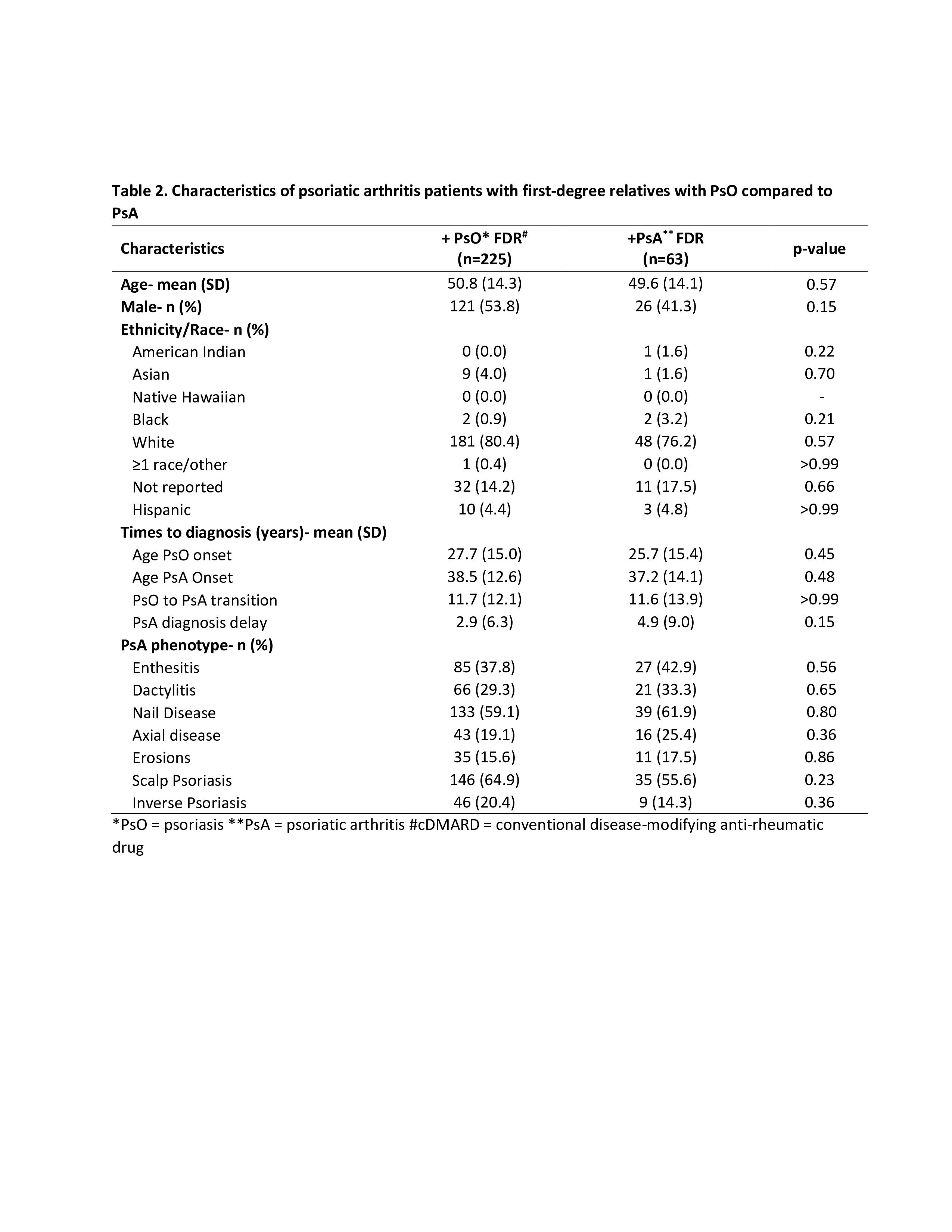
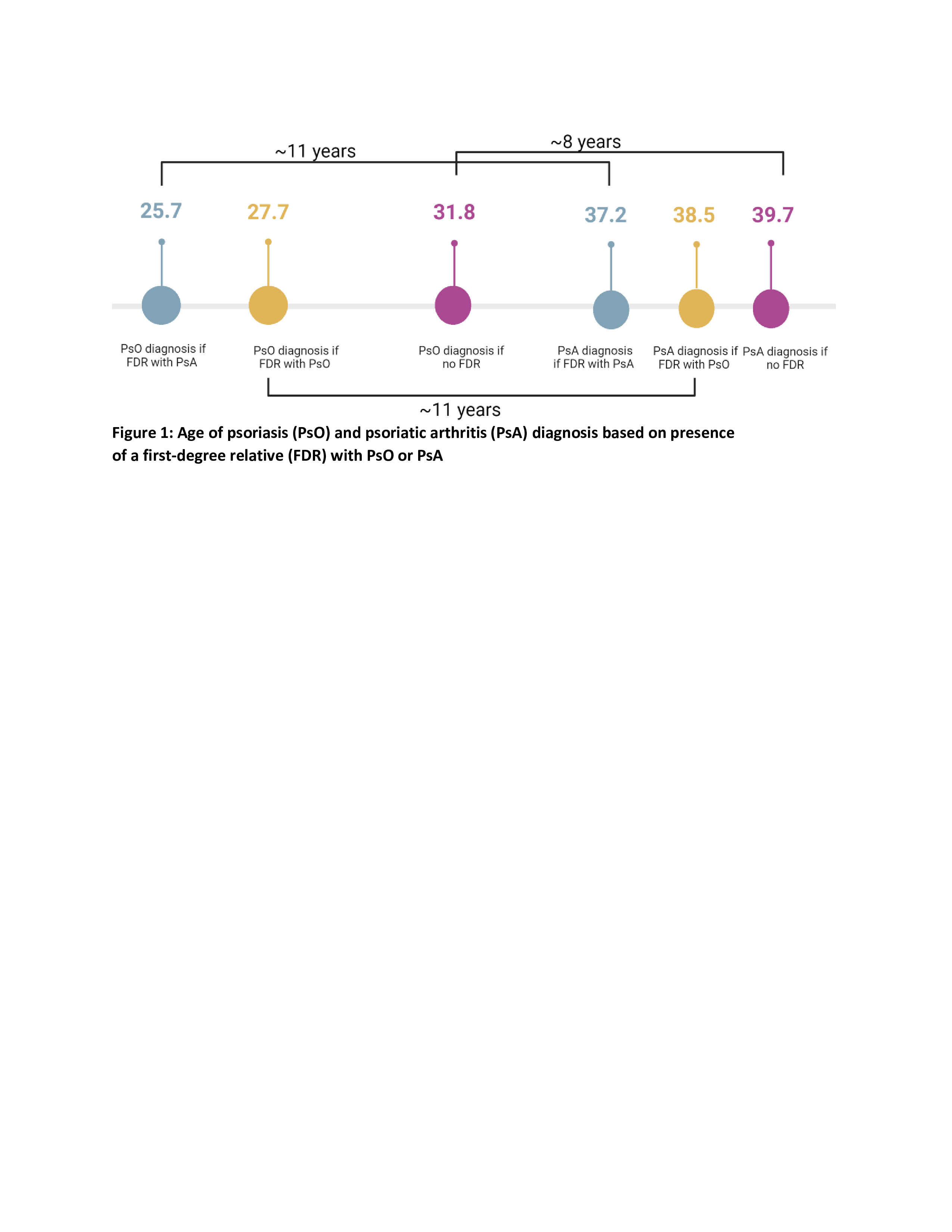
Results: A total of 288 patients (36.3%) had at least one FDR with psoriatic disease (Table 1). Of those, 28.4% had an FDR with PsO and 7.9% had an FDR with PsA (Table 2). Asian patients were less likely to have a family history of psoriatic disease (3.5% with FDR vs. 8.5% without FDR, p < 0.01). Those with a family history developed PsO earlier than those with no family history (27.3 vs. 31.8 years, p < 0.01, Table 1). Although not reaching statistical significance, the mean age of PsA diagnosis was also younger in those with a family history (38.2 vs. 39.7 years, p = 0.16). Furthermore, patients with an FDR with PsA were numerically younger at both PsO and PsA onset compared to those with an FDR with PsO only (25.7 vs. 27.7 years, p=0.45 and 37.2 vs. 38.7, p=0.48; Table 2, Figure 1). The transition time between diagnosis of PsO and PsA was longer among those with a family history (11.7 vs. 8.5 years, p < 0.01), but there was no difference between those with FDRs with PsO and PsA (11.7 vs. 11.6, p > 0.99, Table 2, Figure 1). There were no significant differences in domain involvement based on family history, however, those with an FDR were more likely to have active enthesitis at their baseline visit (31.9% vs. 21.8%, p < 0.01) despite similar medication use (Table 1).
Conclusion: In a single-center psoriatic arthritis cohort, we found that patients with an FDR with psoriatic disease were diagnosed with skin psoriasis earlier and had a trend towards earlier PsA diagnosis. Interestingly, the transition period from PsO to PsA was longer in those with FDRs, although there was no difference in transition time between those with an FDR with PsO compared to PsA. While domain involvement was generally similar between groups, those with a family history had a higher prevalence of enthesitis at their baseline visit. Further research incorporating molecular and immune features is needed to investigate the genetic, environmental and epigenetic factors that may impact the PsA phenotype and severity as well as the transition from psoriasis to PsA.
To cite this abstract in AMA style:
Howe C, Chen W, Hu J, Chen K, Felipe A, Eichman S, Coyle M, Lydon E, Neimann A, Reddy S, Scher J, haberman R. Familial Aggregation in Psoriatic Arthritis: Phenotypic Differences in Patients with and Without First-degree Relatives with Psoriatic Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/familial-aggregation-in-psoriatic-arthritis-phenotypic-differences-in-patients-with-and-without-first-degree-relatives-with-psoriatic-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/familial-aggregation-in-psoriatic-arthritis-phenotypic-differences-in-patients-with-and-without-first-degree-relatives-with-psoriatic-disease/