Session Information
Date: Monday, November 14, 2016
Title: Miscellaneous Rheumatic and Inflammatory Diseases - Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Methods
: This cross-sectional study included all patients diagnosed with UCTD according to the preliminary classification criteria(1), seen at the Columbia University Lupus Center in New York, from January to December 2015. Clinical and immunological variables were ascertained. Chi squared tests were used to compare the following characteristic between treated and untreated patients: demographic characteristics, number of ACR criteria, SLICC criteria, individual symptoms and laboratory values.Results
: Eighty-three patients were identified; 93% were female, mean age at diagnosis of 44 years ±14.9; 67% were Caucasian, 20% Hispanic and 11% Black/African American; median disease duration of 3.91 years±5.35 (1-27). The most prevalent symptoms that required medical attention are described in the Figure 1.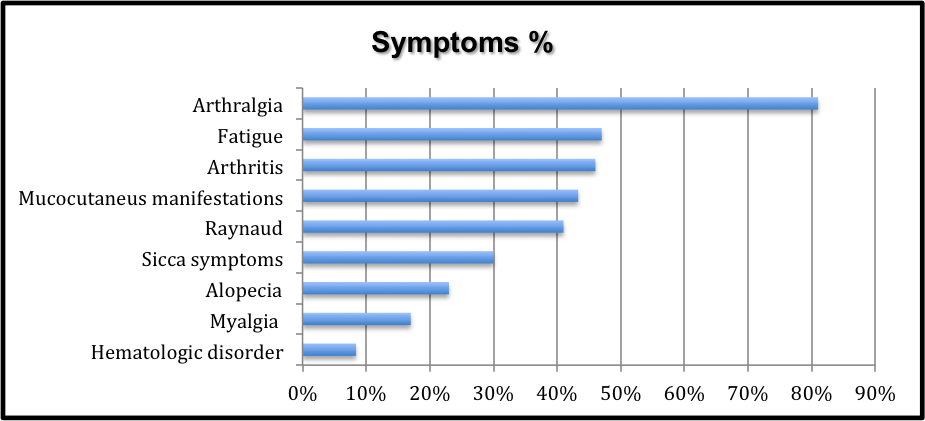
Figure 1. 49.4% of patients had a family history of autoimmune diseases. 95% of patients had positive antinuclear antibody (ANA) titers and 5% were ANA negative Ro/SSA+, 88% had titers ≥ 1:160, with speckled pattern in 69% of patients. 16% of the patients studied met SLICC SLE criteria. Half of the patients, 42(51%) were treated with HCQ and 41(49.3%) were not treated. The patients treated with HCQ were more likely to also meet SLICC criteria (10 vs. 3, respectively; p=0.03), have a history of arthralgia (38 vs. 29; p=0.02), arthritis (28 vs. 10; p=0.0001), and fatigue (25 vs. 14; p=0.02). A history of low complement was more prevalent in the treated group (12 vs. 3; p=0.01). 38 patients had folllow-up greater than 3 years; of these 18 had a strong family history of autoimmune diseases. While only 17(45%) patients had been treated with HCQ, we did not observe any increase in the titer and/or number of autoantibodies or clinical manifestations over the 3 years of follow-up in any of these 38 patients.
Conclusion : Data from this single-center cohort of patients with UCTD show that patients treated with HCQ by their rheumatologist are more likely to have multiple clinical criteria and low complement compared to those that were not treated. These data suggest that rheumatologists treat pre-clinical autoimmunity in the setting of clinical symptoms. None of patients were treated based on serologies alone. Longitudinal studies are needed to evaluate the long-term impact of HCQ on clinical and seologic outcomes of patients with UCTD. References: (1) Mosca M, et al. Undifferentiated connective tissue diseases (UCTD): a review of the literature and a proposal for preliminary classification criteria. Clin Exp Rheumatol 1999;17:615-620.
To cite this abstract in AMA style:
Pena DP, Askanase AD. Factors That Influence Therapy in Patients with Undifferentiated Connective Tissue Disease [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/factors-that-influence-therapy-in-patients-with-undifferentiated-connective-tissue-disease/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-that-influence-therapy-in-patients-with-undifferentiated-connective-tissue-disease/
