Session Information
Date: Tuesday, November 9, 2021
Title: Reproductive Issues in Rheumatic Disorders Poster (1711–1731)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Several prior studies have assessed disease activity in the setting of pregnancy and have shown that certain factors such as thrombocytopenia, systemic lupus erythematosus (SLE) disease activity at pregnancy onset, lupus nephritis, hypertension, antiphospholipid syndrome, and history of preeclampsia are associated with higher rates of SLE flare in pregnancy (1). However, few have focused on the postpartum period and have shown varying results. While some studies showed an increase in flares in the postpartum period (2-4), others showed no flares in the postpartum period (5). The objective of this study was to identify factors associated with the occurrence of SLE flares in the 6-month postpartum period. Identifying these factors is important for stratifying and monitoring lupus patients in the postpartum period.
Methods: Lupus pregnancies were retrospectively identified via chart review at a tertiary care center in New York from 2005 – 2020. Flares in the 6-month postpartum period were physician reported, as documented in the patient chart by the treating rheumatologist, or identified by an escalation in medication regimen.
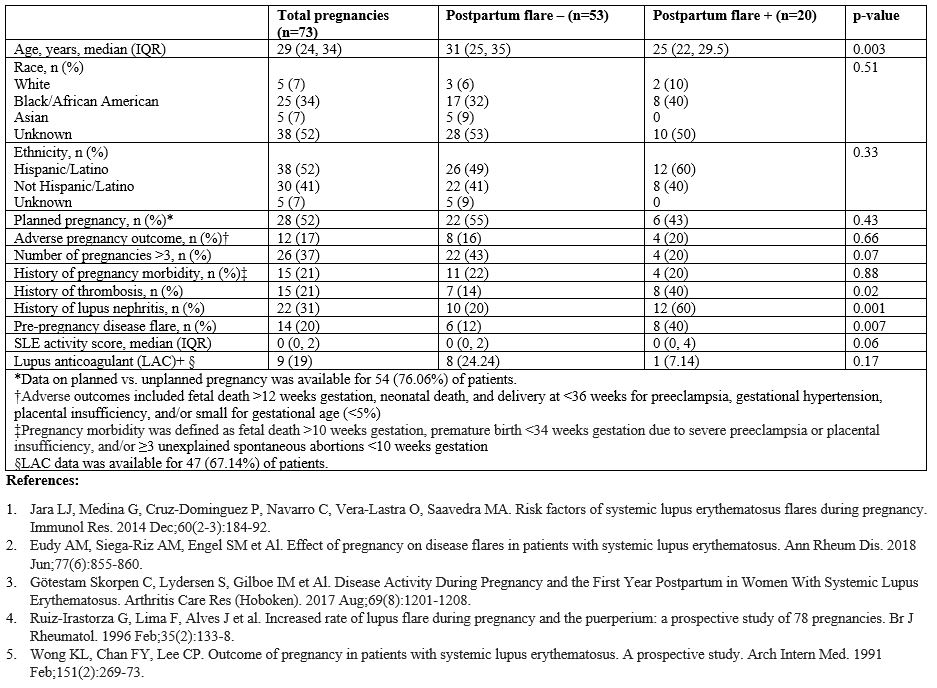
Results: Of the 103 lupus pregnancies reviewed, 73 pregnancies had documented follow up in the 6-month postpartum period, of which 20 (27%) were identified to have had SLE flares. This sample was representative of the overall population of pregnant women at our center. The median (IQR) age of the patient population was 29 (24, 34) years old. Thirty-eight (52%) patients self-identified as Hispanic or Latina, 25 (34%) as Black or African American, 5 (7%) as Asian and 5 (7%) as Caucasian (Table). Patients with postpartum flare were more likely to have history of thrombosis (40% vs 14%, p=0.02), lupus nephritis (60%, vs 20%, p=0.001), and SLE flare in the 6 months prior to conception (40% vs 12%, p=0.007) when compared to those without flare. Women who experience postpartum flares were younger (median IQR) [25 (22, 30) years old vs 31 (25, 35) years old, p=0.003] and more likely to have fewer than 3 total pregnancies (80% vs 57%, p=0.07). The median (IQR) SLEPDAI score amongst those with postpartum flare was higher in comparison to those without [2 (0, 4) vs 0 (0, 2), respectively, (p=0.06)]. Pre-pregnancy flares were associated with postpartum flares even after adjusting for SLEPDAI during pregnancy (OR 4.4, CI 1.15-16.81, p=0.03). Ethnicity, adverse pregnancy outcomes, pregnancy morbidity, and planned vs unplanned pregnancy were not associated with postpartum flare.
Conclusion: This study shows that younger women with fewer total pregnancies, history of thrombosis, lupus nephritis, and active disease prior to conception should be closely monitored for postpartum flare. Patients with these characteristics can be risk stratified and should be counseled appropriately to monitor for signs of flare in the postpartum period.
 Factors Related to Post-pregnancy Lupus Flare
Factors Related to Post-pregnancy Lupus Flare
To cite this abstract in AMA style:
Ramu A, Veyseh M, Lally B, Wang S, Broder A. Factors Associated with Postpartum Flare in Women with Lupus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-postpartum-flare-in-women-with-lupus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-postpartum-flare-in-women-with-lupus/
