Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Pauci-immune glomerulonephritis (GN) is a renal manifestation of anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV). When patients present with positive ANCA results and urinary abnormalities such as hematuria and proteinuria, pauci-immune GN is suspected. However, some patients with positive ANCA results have renal pathologies other than pauci-immune GN. Thus, this study aimed to investigate and compare the characteristics of patients with positive ANCA results who were diagnosed with pauci-immune GN with those with other renal pathologies based on renal tissue examination.
Methods: We retrospectively reviewed the electronic medical records of patients who underwent renal biopsy with positive ANCA results from January 2010 to October 2023 at a single tertiary center in Seoul, South Korea. Logistic regression analysis was performed to identify the variables associated with pauci-immune GN.
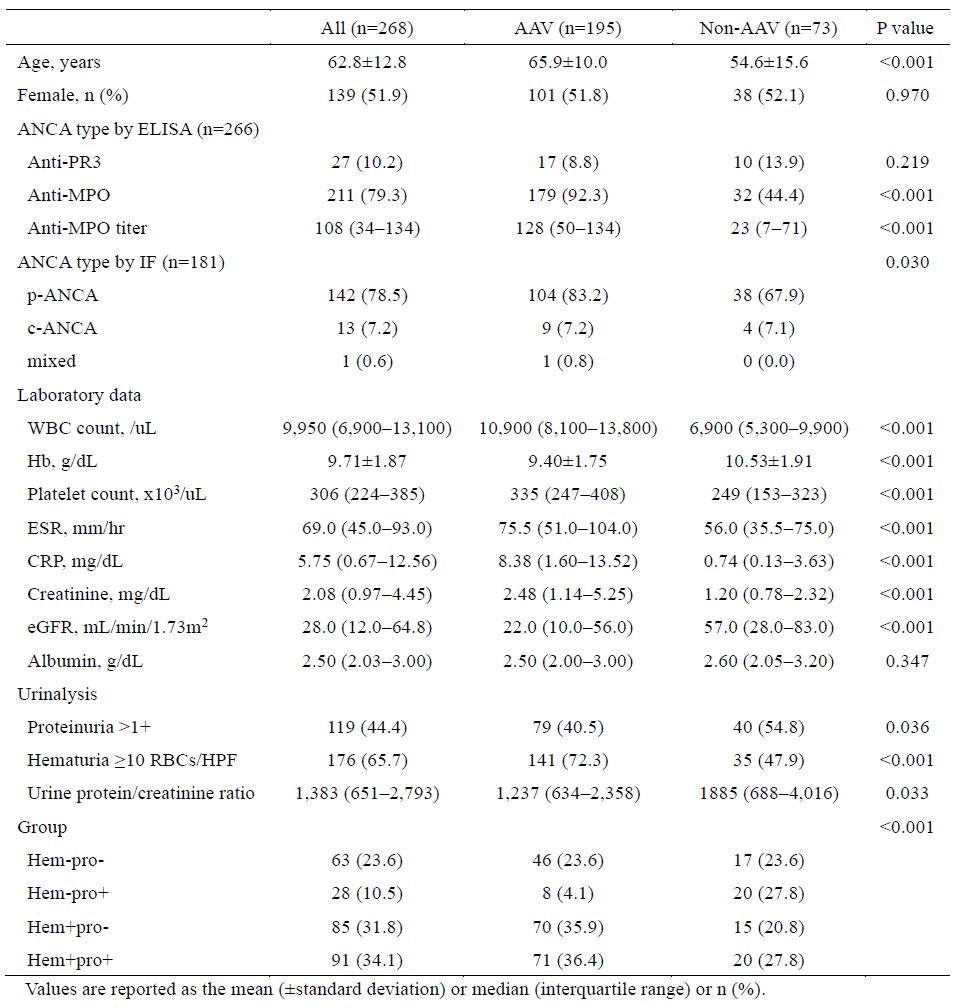
Results: A total of 268 patients with positive ANCA results who underwent renal biopsy were included in our analysis (Table 1). The mean age was 62.8±12.8 years, and 51.9% were female. Of all patients, 195 (72.8%) were diagnosed with pauci-immune GN, while 73 (27.2%) were diagnosed with other kidney diseases. The non-pauci-immune GN group exhibited diverse pathological findings, and the most prevalent conditions were IgA nephritis (20.6%), lupus nephritis (17.5%), membranous glomerulonephritis, and diabetic nephropathy.
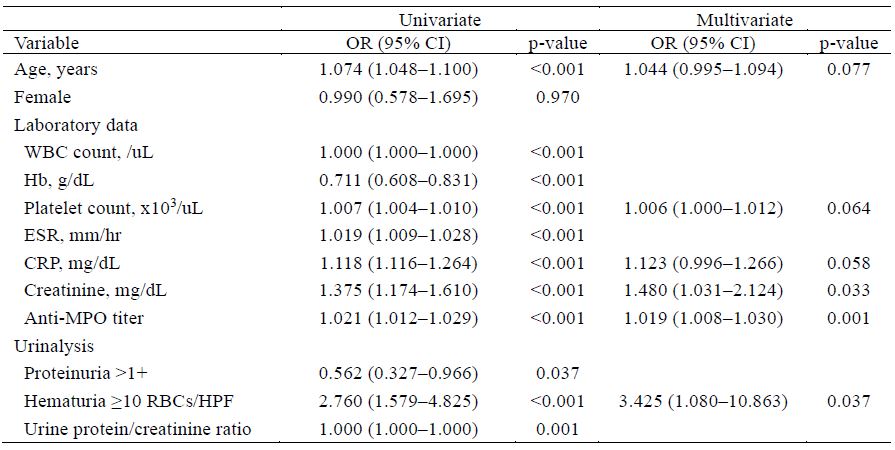
In the analysis of differences between pauci-immune GN and non-pauci-immune GN, the pauci-immune GN group had a higher mean age (65.9 vs. 54.6 years, p< 0.001) than the non-pauci-immune GN group. Anti-myeloperoxidase (MPO) positivity was significantly higher in the pauci-immune GN group than in the non-pauci-immune GN group (92.3% vs. 44.4%, p< 0.001), with a median anti-MPO titer of 128 IU/mL vs. 23 IU/mL. The pauci-immune GN group also showed a statistically significantly higher white blood cell count, platelet count, erythrocyte sedimentation rate, C-reactive protein level, and creatinine level and lower hemoglobin levels than the non-pauci-immune GN group. Proteinuria was less common, while hematuria was more common on urinalysis in the pauci-immune GN group. Multivariate analysis identified significant associations between anti-MPO titer (OR: 1.019), creatinine levels (OR: 1.480) and hematuria (OR: 3.425) with pauci-immune GN on renal tissue examination (Table 2).
Conclusion: In this cohort, approximately 70% of patients who underwent renal biopsy and tested positive for ANCA were diagnosed with pauci-immune GN. Significant predictive factors for pauci-immune GN included anti-MPO titer, creatinine levels, and microscopic hematuria. These findings emphasize the importance of identifying high-risk laboratory data, and urinalysis results associated with AAV.
To cite this abstract in AMA style:
Lee J, Lee Y, Cho M, Kim Y, Ahn S, Oh J, Kim Y, Lee C, Yoo B, Hong S. Factors Associated with Pauci-immune Glomerulonephritis in Patients Undergoing Renal Biopsy with Positive ANCA Results [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-pauci-immune-glomerulonephritis-in-patients-undergoing-renal-biopsy-with-positive-anca-results/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-pauci-immune-glomerulonephritis-in-patients-undergoing-renal-biopsy-with-positive-anca-results/