Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Achieving minimal disease activity (MDA) is an important treatment goal in psoriatic arthritis (PsA), as it leads to improved clinical outcomes and quality of life for patients. However, the impact of specific clinical factors and therapies on long-term MDA status requires further investigation. The aim of this study was to identify treatment factors associated with minimal disease activity (MDA) status in PsA patients.
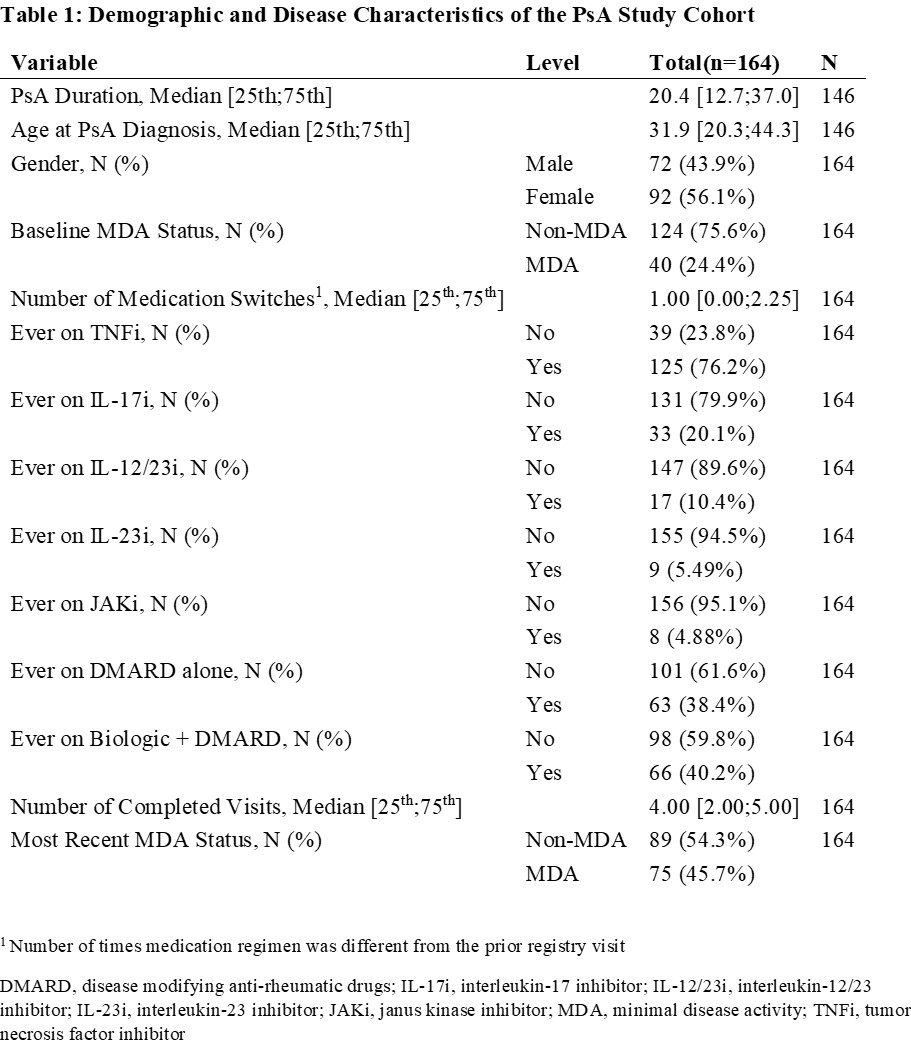
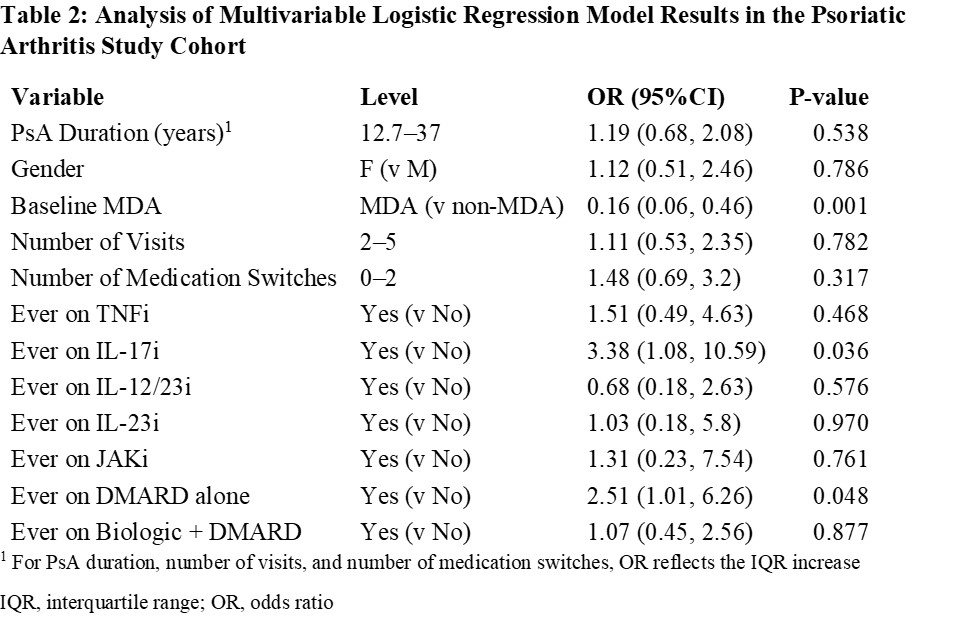
Methods: We utilized data from a tertiary care psoriatic disease biorepository, collecting patient- and physician-reported outcomes and clinical information longitudinally. Adult PsA in the registry for more than one year with at least two evaluations of MDA status were included. A multivariable logistic regression model was constructed to investigate factors associated with long-term MDA status. Candidate predictors included: PsA duration (at the most recent recorded visit), gender, baseline MDA status, number of completed visits in the registry, number of medication regimen switches, and seven medication class-related variables (use of TNFi, IL-17i, IL-12/23i, IL-23i, JAKi, oral DMARD only, and combination biologic and oral DMARD). The outcome of interest was long-term MDA status, defined MDA status at the most recent registry visit. Continuous variables were summarized using medians and IQR, while categorical variables were summarized using counts and frequencies. Model results were presented using odds ratios and 95% confidence intervals for likelihood of being in non-MDA status at the most recent registry visit. All tests were two-sided, assuming an alpha level of 0.05.
Results: The analysis included 164 PsA patients with an average duration of PsA of 20.4 years, of whom 56% were female. Approximately 75% of patients were not in MDA at baseline, while approximately 54% of patients were not in MDA at their most recent evaluation. Baseline MDA status showed the most significant association with long-term MDA status. Patients in MDA at baseline had an 84% lower likelihood of being in non-MDA status at their most recent evaluation compared to patients not in MDA at baseline (OR 0.16, 95% CI: 0.06, 0.46, p = 0.001). In other words, patients in MDA at baseline were much more likely to be in MDA long-term. The use of IL-17 inhibitors (OR 3.38, 95% CI: 1.08, 10.59, p = 0.036) or oral DMARDs alone (OR 2.51, 95% CI: 1.01, 6.26, p = 0.048) during the registry period decreased the likelihood of long-term MDA status. No other medication or continue variable had a significant effect on the final MDA status.
Conclusion: This registry-based study provides insights into factors associated with minimal disease activity in PsA patients. Baseline MDA status is a key predictor of long-term MDA status, emphasizing the importance of achieving early MDA. The use of IL-17 inhibitors and oral DMARD alone were associated with a decreased likelihood of achieving MDA. These findings can assist in risk stratification and guide clinicians in selecting therapies for improved psoriatic disease control.
To cite this abstract in AMA style:
Cheemalavagu S, Jin Y, Husni M. Factors Associated with Minimal Disease Activity in Psoriatic Arthritis: Insights from a Registry-Based Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-minimal-disease-activity-in-psoriatic-arthritis-insights-from-a-registry-based-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-minimal-disease-activity-in-psoriatic-arthritis-insights-from-a-registry-based-study/