Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Early hospital readmission is a major healthcare burden. Studies evaluating factors associated with readmissions in rheumatic diseases are sparse. Our aim was to use a large national database to identify rates and the predictors of readmission in SLE as compared to common medical conditions with known high readmission rates including congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD).
Methods: We used the US nationwide readmission database (NRD, 2010-2014) to identify index adult (≥ 18 years) discharges with SLE, CHF, and COPD using ICD-9 codes in the first 5 diagnosis positions, and assessed their rates of readmission (defined as “early” readmission within 30 days). Index discharges with same-day transfers or those discharged as deceased were excluded. Discharges with the same diagnosis after 30 days from the previous index discharge date could count as another index, thus, allowing one patient to contribute to multiple observations. We performed multivariate regression to identify factors independently associated with early readmission, including demographic, hospital, and clinical factors. Comorbidities that were significant in univariate analysis (p≤0.05) were included in the multivariate model. We accounted for the clustering of multiple index discharges within the same patient using generalized estimating equations.
Results: In the combined data from 2010-2014, we identified 351,219 index SLE discharges, and compared them to 3,022,240 CHF, and 4,052,574 COPD index discharges. The readmission rate was 16.9% for SLE compared to 21.3% for CHF and 18.4% for COPD. Readmission was higher in males (19.5 %, 21.4 % and 19.4%) compared to females (16.6%, 21.2% and 17.7 %) for SLE, CHF and COPD, respectively.
Some demographic and hospital factors associated with higher odds of readmission in SLE included non-private insurance, longer length-of-stay at index hospitalization, and lowest income quartile. Age >65 and female sex were associated with reduced odds of readmission. Discharges against medical advice (AMA) had a higher odds of readmission in all cohorts (Table 1).
Among select diagnoses present in the index SLE discharges, the top 5 comorbid conditions associated with highest odds of readmission were chronic kidney disease (OR: 1.31, 95% CI: 1.23 – 1.39, p< 0.001), alcoholic liver disease (OR: 1.30 , 95% CI: 1.02 -1.65, p=0.03), anemia (OR 1.24, 95% CI: 1.20 – 1.28, p< 0.001) , coagulation disorders (OR: 1.19, 95% CI 1.14 – 1.25, p< 0.001), and CHF (OR: 1.17, 95% CI: 1.11– 1.23, p< 0.001). Acute kidney injury was associated with early readmission in CHF and SLE. Carditis (peri-, myo- and endocarditis) and cardiomyopathy were associated with increased readmission only in SLE (Fig 1).
Conclusion: We found readmission in SLE to be comparable to that in CHF and COPD. Higher readmission in younger SLE patients likely reflects the more severe phenotype in this group. Similarly, the presence of anemia, coagulopathy, and myopericarditis conferred higher readmission risk, likely reflecting more severe SLE with organ involvement. Studying the role of various common and unique predictors in a prospective setting could identify avenues for improving inpatient and transitional care in SLE.
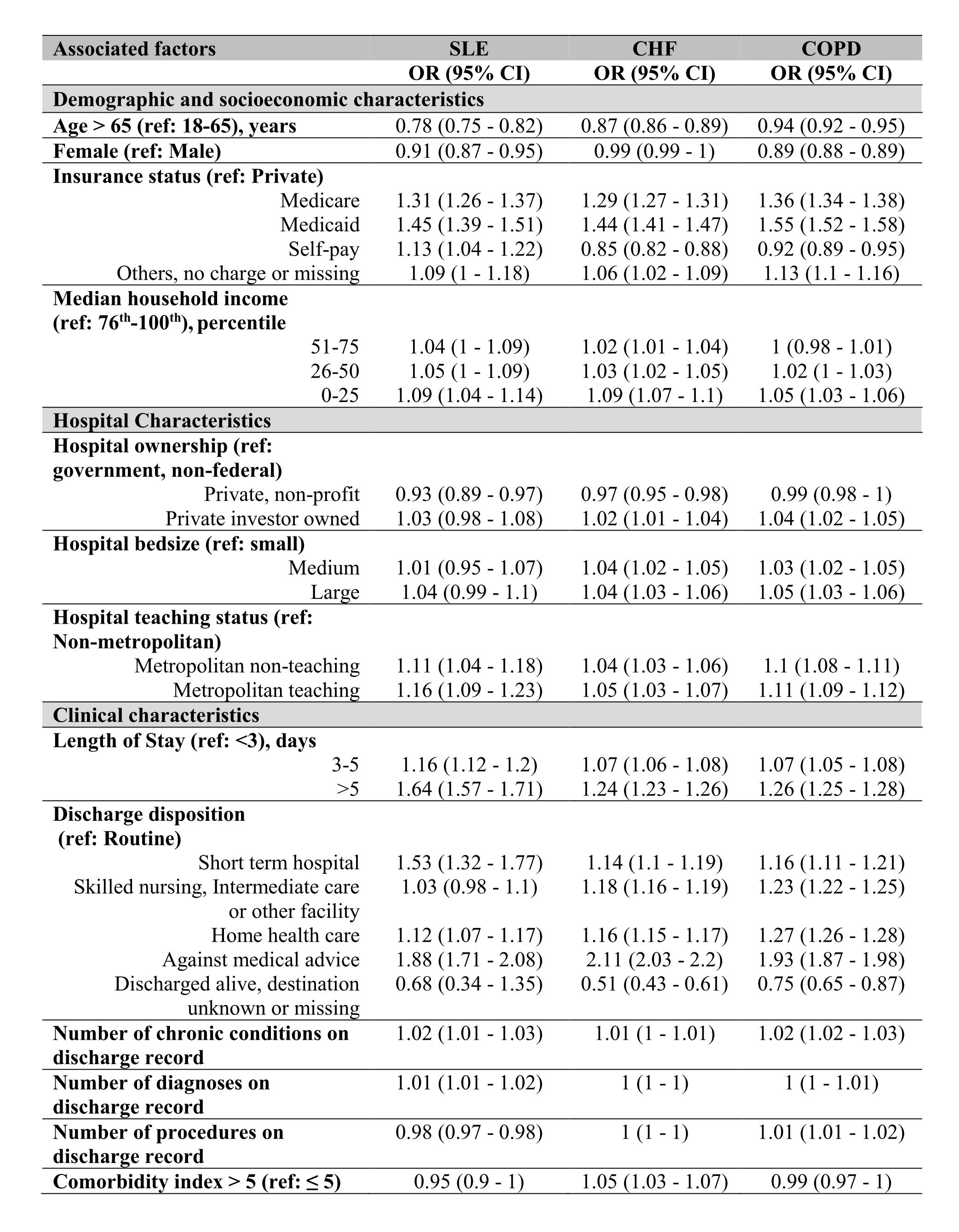 Table 1: Multivariate analysis of demographic, hospital and clinical factors associated with early readmission in systemic lupus erythematosus (SLE), congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD)
Table 1: Multivariate analysis of demographic, hospital and clinical factors associated with early readmission in systemic lupus erythematosus (SLE), congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD)
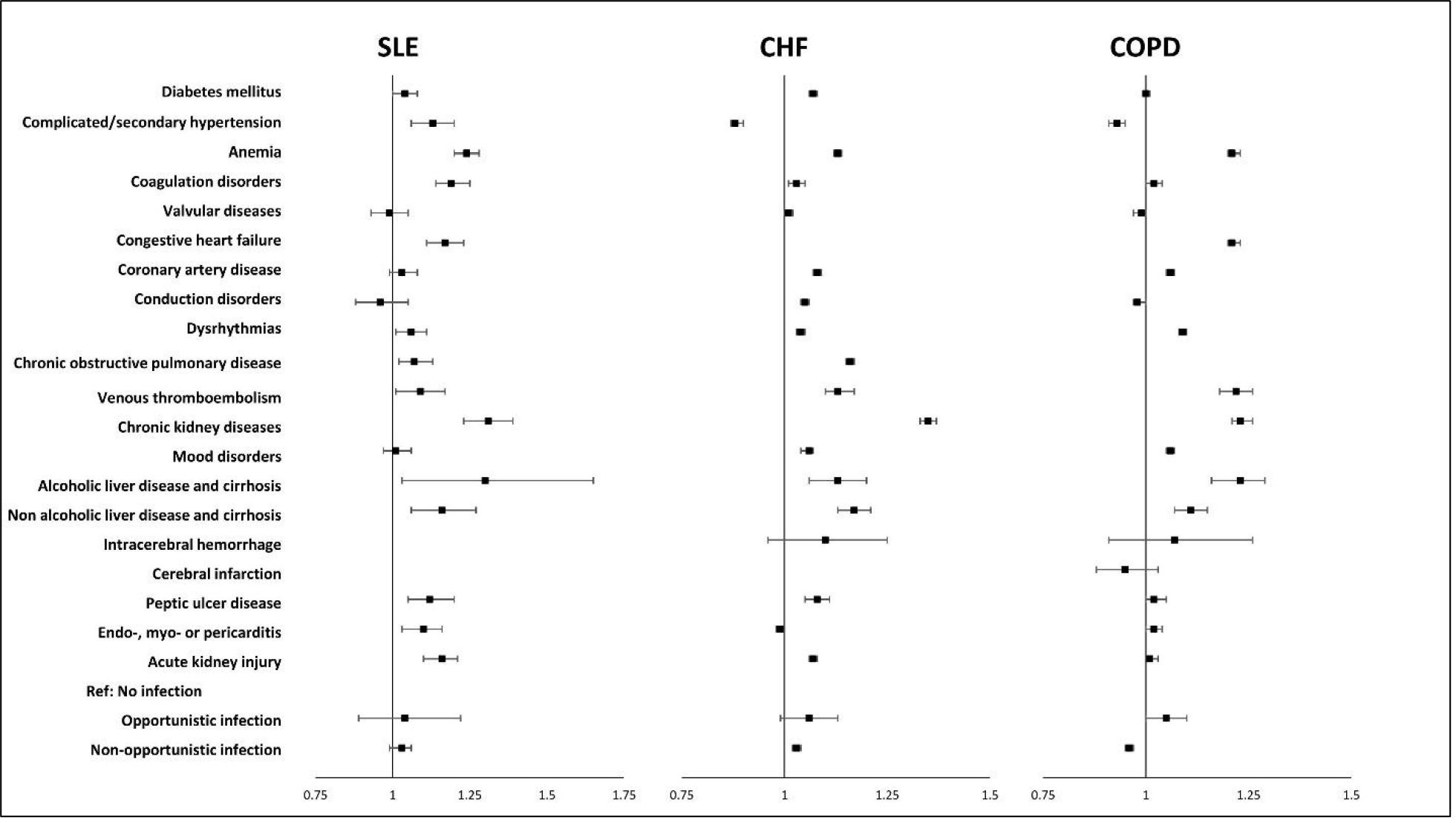 Figure 1: Multivariate analysis of comorbidities present at index discharges associated with early readmission in systemic lupus erythematosus (SLE), congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD)
Figure 1: Multivariate analysis of comorbidities present at index discharges associated with early readmission in systemic lupus erythematosus (SLE), congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD)
To cite this abstract in AMA style:
Dhital R, Baker J, Karmacharya P, Donato A, Poudel D. Factors Associated with Early Hospital Readmission in Systemic Lupus Erythematosus: Data from National Readmission Database [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/factors-associated-with-early-hospital-readmission-in-systemic-lupus-erythematosus-data-from-national-readmission-database/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-early-hospital-readmission-in-systemic-lupus-erythematosus-data-from-national-readmission-database/
